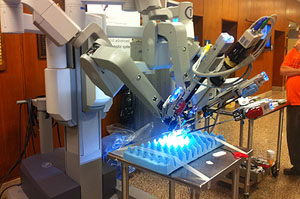
In the dozen years since the Da Vinci robot has been approved for surgeries in the United States, it’s been embraced by health care providers and patients alike. Surgeons routinely use the multi-armed metal assistant to remove cancerous prostate glands and uteruses, repair heart valves and perform gastric bypass operations, among many other procedures.
Lately a key study and reports of problems have raised questions about robotic surgery’s safety and cost-effectiveness, leading to a review of the Da Vinci system by the Food and Drug Administration and causing some experts to wonder whether the benefits of undergoing robot-assisted surgery may have been overstated.
At this time, health insurers generally pay for robotic surgery just as they would any other surgical procedure, and patient out-of-pocket costs are typically no different either. That could change, some say, as more comprehensive data become available that clarifies when robotic-assisted surgery helps improve patient outcomes—and when it doesn’t.
Robotic surgery is similar to conventional laparascopic surgery, in which surgical instruments are inserted into small incisions in a patient’s torso and manipulated by the surgeon. In robotic surgery, however, the surgeon sits at a console in the operating room and uses hand and foot controls to manipulate surgical tools attached to a robot’s arms. Both types of surgery may result in quicker recovery times, less blood loss and pain for patients compared with traditional “open” surgeries performed through a larger incision.
Robot-assisted surgeries are generally more expensive than other methods, however, and don’t necessarily improve patient outcomes long-term. A study published in February in the Journal of the American Medical Association of more than 260,000 hysterectomy patients found that the median hospital cost for robot-assisted surgery was $8,868, compared with $6,679 for a laparascopic hysterectomy. The study found that although patients who got robotic hysterectomies were less likely than laparscopic patients to be hospitalized for more than two days, there was no significant difference between the two groups on other measures, such as complications and blood transfusion rates.
In March, the American Congress of Obstetricians and Gynecologists released a statement that said in part, “There is no good data proving that robotic hysterectomy is even as good as—let alone better—than existing, and far less costly, minimally invasive alternatives.” The statement said that conventional laparascopic hysterectomy and a procedure performed through an opening at the top of the vagina have proven track records and were generally preferable to robotic hysterectomy. That statement, however, was assailed by other physicians who use the robot.
“Our study and the ACOG statement raise awareness that we really need to be critical. Robotic hysterectomy may not be the best procedure from a patient’s perspective,” says Jason Wright, an assistant professor of women’s health at Columbia University College of Physicians and Surgeons and the lead author of the study.
“Patients need factual information about all of their treatment options, and the evidence supports that robotic surgery has dramatically decreased the number of open hysterectomies in the U.S.,” says Angela Wonson, a spokesperson for Intuitive Surgical, the manufacturer of the Da Vinci system. “Robotic surgery is a technological advance that is enabling more women to receive minimally invasive surgery.”
A 2010 New England Journal of Medicine analysis of studies that examined 20 robot-assisted procedures found that using a robot added about 13 percent, or $3,200, to the average cost of a procedure in 2007. The authors noted that there were no large-scale randomized trials of robot-assisted surgery and that the limited data available failed to show that robot-assisted surgery was superior to other procedures.
The lack of hard data hasn’t stopped patients, their doctors and hospitals from enthusiastically adopting robotic surgery. Nearly a quarter of hospitals offered robotic surgery in 2011, according to the American Hospital Association. Last year, 367,000 robotic procedures were performed in the United States using da Vinci robots, according to Intuitive Surgical, a 26 percent increase over the 292,000 procedures performed the previous year.
John Bello, 48, had his cancerous prostate gland removed robotically two years ago by a surgeon at MedStar Washington Hospital Center in the District. The Annapolis resident couldn’t be happier with the results of the surgery, which was covered without a hitch by his Blue Cross Blue Shield plan. Although many patients struggle with impotence or incontinence following prostate cancer surgery, Bello says he has not had any serious side effects from the surgery. He’s cancer free.
“Unless I see the scars … I don’t even think about it,” he says.
To date, hospitals, eager to attract patients with the technology du jour, have generally been willing to absorb the higher costs associated with robotic surgery. But health care overhaul provisions that encourage payments to providers based on “episodes of care” rather than individual services may begin to change these practices, say experts.
“As we move away from the fee-for-service model, we’re going to discourage [procedures] that are no better than the higher priced one,” says A. Mark Fendrick, director of the Center for Value-Based Insurance Design at the University of Michigan.
“Health plans will try to incentivize the appropriate surgery, and that is especially true with the evolving payment models that reward quality outcomes,” says Susan Pisano, a spokeswoman for America’s Health Insurance Plans, a trade group.
This article was produced by Kaiser Health News with support from The SCAN Foundation.
Please send comments or ideas for future topics for the Insuring Your Health column to questions@kffhealthnews.org.