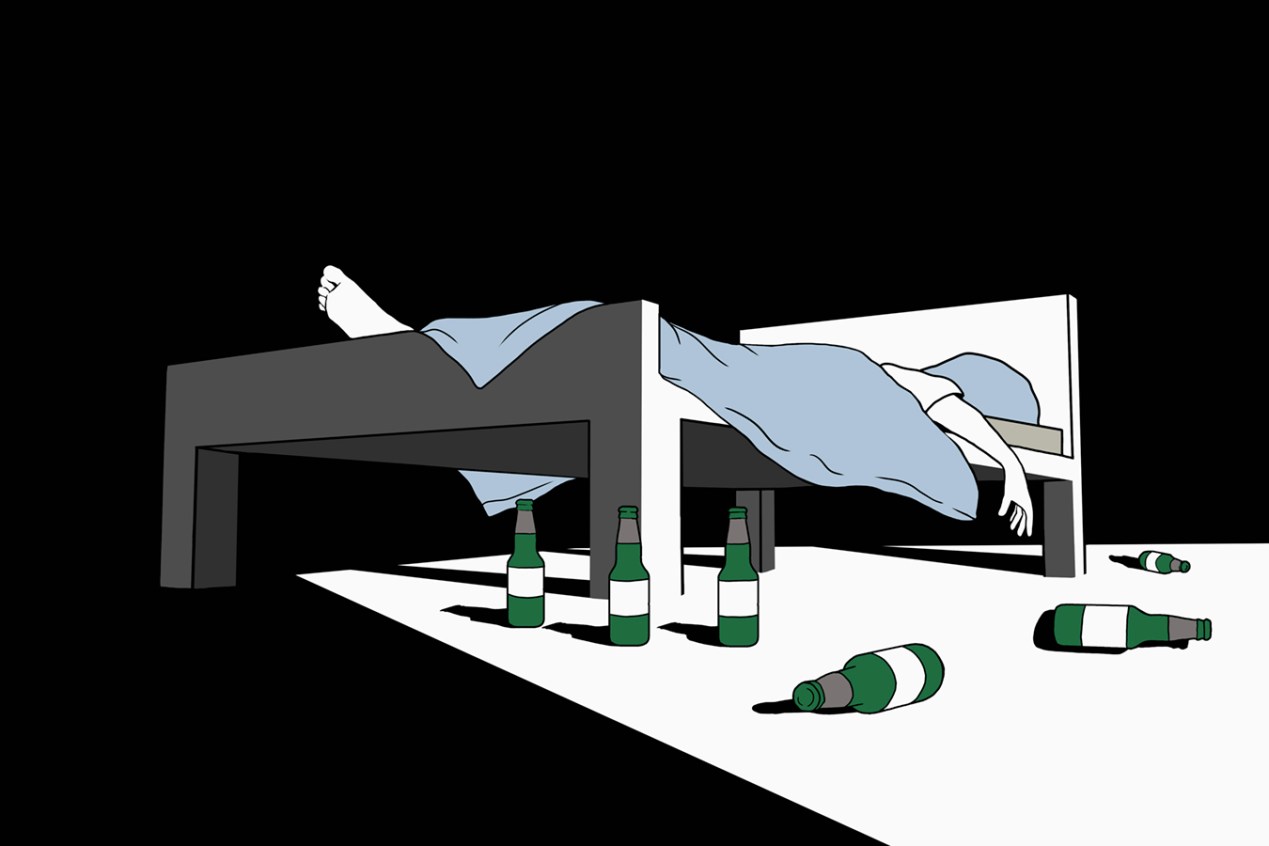
As the pandemic sends thousands of recovering alcoholics into relapse, hospitals across the country have reported dramatic increases in alcohol-related admissions for critical diseases like alcoholic hepatitis and liver failure.
Alcoholism-related liver disease was a growing problem even before the pandemic, with 15 million people diagnosed with the condition around the country, and with hospitalizations doubling over the past decade.
But the pandemic has dramatically added to the toll. Although national figures are not available, admissions for alcoholic liver disease at Keck Hospital of the University of Southern California were up 30% in 2020 compared with 2019, said Dr. Brian Lee, a transplant hepatologist who treats the condition in alcoholics. Specialists at hospitals affiliated with the University of Michigan, Northwestern University, Harvard University and Mount Sinai Health System in New York City said rates of admissions for alcoholic liver disease have leapt by up to 50% since March.
High levels of alcohol ingestion lead to a constellation of liver diseases due to toxic byproducts associated with the metabolism of ethanol. In the short term, these byproducts can trigger extensive inflammation that leads to hepatitis. In the long term, they can lead to the accumulation of fatty tissue, as well as the scarring characteristic of cirrhosis — which can, in turn, cause liver cancer.
Since the metabolism of alcohol varies among individuals, these diseases can show up after only a few months of heavy drinking. Some people can drink heavily without experiencing side effects for a long time; others can suffer severe immune reactions that rapidly send them to the hospital.
Leading liver disease specialists and psychiatrists believe the isolation, unemployment and hopelessness associated with covid-19 are driving the explosion in cases.
“There’s been a tremendous influx,” said Dr. Haripriya Maddur, a hepatologist at Northwestern Medicine. Many of her patients “were doing just fine” before the pandemic, having avoided relapse for years. But subject to the stress of the pandemic, “all of a sudden, [they] were in the hospital again.”
Across these institutions, the age of patients hospitalized for alcoholic liver disease has dropped. A trend toward increased disease in people under 40 “has been alarming for years,” said Dr. Raymond Chung, a hepatologist at Harvard University and president of the American Association for the Study of Liver Disease. “But what we’re seeing now is truly dramatic.”
Maddur has also treated numerous young adults hospitalized with the jaundice and abdominal distension emblematic of the disease — a pattern she attributes to the pandemic-era intensification of economic struggles faced by the demographic. At the same time these young adults may be entering the housing market or starting a family, entry-level employment, particularly in the vast, crippled hospitality industry, is increasingly hard to come by. “They have mouths to feed and bills to pay, but no job,” she said, “so they turn to booze as the last coping mechanism remaining.”
Women may be suffering disproportionately from alcoholic liver disease during the pandemic because they metabolize alcohol at slower rates than men. Lower levels of the enzyme responsible for degrading ethanol leads to higher levels of the toxin in the blood and, in turn, more extensive organ damage in women than in men who drink the same amount. (The CDC recommends that women have one drink or less per day, compared with two or fewer for men.)
Socially, the “stress of the pandemic has, in some ways, particularly targeted women,” said Dr. Jessica Mellinger, a hepatologist at the University of Michigan. Lower wages, less job stability and the burdens of parenting tend to fall more heavily on women’s shoulders, she said.
“If you have all of these additional stressors, with all of your forms of support gone — and all you have left is the bottle — that’s what you’ll resort to,” Mellinger said. “But a woman who drinks like a man gets sicker faster.”
Nationwide, more adults are turning to the bottle during the pandemic: One study found rates of alcohol consumption in spring 2020 were up 14% compared with the same period in 2019 and drinkers consumed nearly 30% more than in pre-pandemic months. Unemployment, isolation, lack of daily structure and boredom all have increased the risk of heightened alcohol use.
“The pandemic has brought out our uneasy relationship with alcohol,” said Dr. Timothy Fong, an addiction psychiatrist at UCLA. “We’ve welcomed it into our homes as our crutch and our best friend.”
These relapses, and the hospitalizations they cause, can be life-threatening. More than 1 in 20 patients with alcohol-related liver failure die before leaving the hospital, and alcohol-related liver disease is the leading cause for transplantation.
The disease also makes people more susceptible to covid: Patients with liver disease die of covid at rates three times higher than those without it, and alcohol-associated liver disease has been found to increase the risk of death from covid by an additional 79% to 142%.
Some physicians, like Maddur, are concerned the stressors leading to increased alcohol consumption and liver disease may stretch well into the future — even after lockdowns lift. “I think we’re only on the cusp of this,” she said. “Quarantine is one thing, but the downturn of the economy, that’s not going away anytime soon.”
Others, like Lee, are more optimistic — albeit cautiously. “The vaccine is coming to a pharmacy near you, covid-19 will end, and things will begin to get back to normal,” he said. “But the real question is whether public health authorities decide to act in ways that combat [alcoholic liver disease].
“Because people are just fighting to cope day to day right now.”
This story was produced by KHN, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.