Politics are more polarized and acrimonious than ever. But one public health concern — the nation’s epidemic of prescription painkiller abuse — is uniting some unexpected bedfellows.
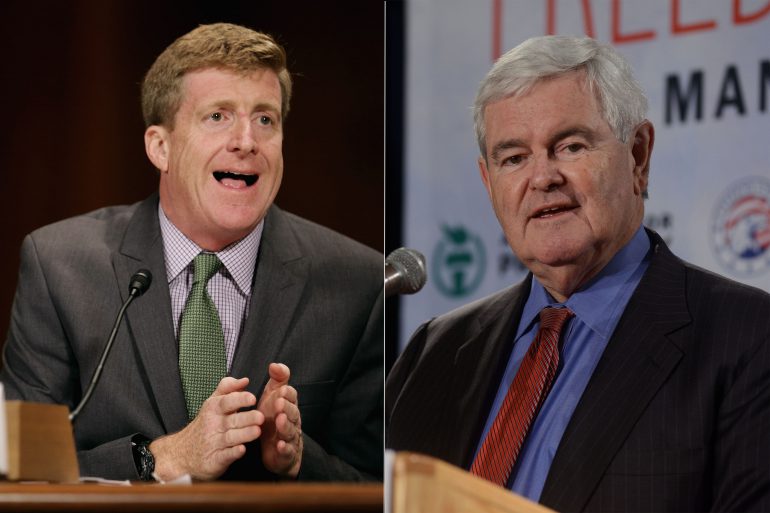
There is Patrick Kennedy, former Democratic congressman from Rhode Island, who has since made a career of advocating for mental health treatment since leaving the House in 2011. And there is Newt Gingrich, the former Republican speaker of the House of Representatives and 2012 presidential candidate, who recently has been mentioned as a possible vice presidential pick for Donald Trump.
The two, however, are quick to point out that, back in their Capitol Hill days, they had a history of working together.
Now, joining forces with criminal justice advocate Van Jones, the pair is pushing for policy changes that would shift how the health system treats addiction and how that treatment is financed, such as allowing more doctors to prescribe opioid reduction therapy — in which doctors give patients smaller amounts of less addictive drugs — and making insurance plans pay more generously for that kind of care.
Kennedy and Gingrich recently spoke with KHN’s Shefali Luthra about why the issue of opioid addiction is gaining traction, what’s needed from Congress and how efforts to treat the opioid epidemic could fit into broader efforts to improve mental health care.
The conversation has been edited for length and clarity.
Q: Why suddenly is opioid addiction an issue people are talking about?
Gingrich: What struck me was when the number of addiction deaths passed the number of people who died in automobile accidents. You realize finally … [there have been] real medical breakthroughs that dramatically transform the number of people [with addictions] whose lives can be saved. That’s the critical mass: The size of the problem combined with the fact that the size of the solution now can potentially match the problem.
Q: Why do you think this seems like an area in which bipartisan action could occur? Do you think we will see real change?
Kennedy: To address that — this is not just kind of a “bipartisan issue” in a small sense. It’s a much bigger issue. Even though you have bipartisan efforts in Congress, they can still be bipartisan and be insufficient, right? The bills currently in Congress really don’t hold a candle to the problem. (Currently, legislation pending on Capitol Hill would fund treatment in areas hard-hit by the epidemic and bolster access to drugs like Naloxone, which reverses overdoses.)
Q: When you say that the Congressional approach falls short, what steps are necessary?
Kennedy: Opioid replacement therapy is the standard evidence-based model to treat people with acute opioid addiction, and that is unassailable according to every research study that’s been done. If that is the evidence-based model, then why can’t we meet the large-scale need that’s out there? We can’t because one, there aren’t enough doctors who can prescribe [drugs like methadone], and two, there are these artificial limits [by insurers] on who doctors can prescribe to.
Our contention is not that medication alone is the answer. We really need to have it in conjunction with cognitive behavioral therapy and with peer support. And that needs to be reimbursed [by health insurers], because it shows huge reductions in overall spending.
You need a comprehensive approach to helping people.
Gingrich: There are whole states where people [with addiction or mental health issues] can’t get to a doctor. If that were true of pancreatic cancer, if that were true of heart disease, if that were true of diabetes, we’d all understand that it made no sense at all. And yet we somehow approach mental health from a very different standard.
Q: The White House has been looking for about $1 billion in funding to combat opioid addiction. It seems that, so far, the proposed congressional appropriations fall short. Do you think that that lack of funding could make a difference?
Gingrich: [We] need the level of investment. I get very frustrated when I look at a one-sided accounting. If I can get you to a point where you can lead a full life, sustain a job, earn money for your family — you can be completely engaged as a citizen. All of these achievements ought to be counted as part of the equation.
Kennedy: The bottom line is, we can’t fight this disease on grants. You don’t fight cancer with grants, or heart disease with grants. We may need some grants to obviously prop up a system that has been underfunded for so long.
But what we really need … is a fundamental paradigm shift that treats this in the way of all other diseases. And that’s the kind of reimbursement that would be necessary for any other chronic illness: diabetes, cardiovascular disease and so forth. That’s going to take more than a congressional appropriations cycle. It’s going to take a fundamental reform in the way we pay for these things.
Q: Another issue is that of excessive prescribing. Is that something you are concerned about?
Gingrich: When we have laws that compartmentalize medical information, and when we have paper systems that compartmentalize medical information, you sometimes have a doctor who understands his specialty and is terrific on your kidneys, but he doesn’t understand the totality of who you are. He may prescribe something where, if he understood completely who you were, he may never consider prescribing [opioids].
We have to rethink, how do we get a complete 360-degree understanding of the patient? So we have genuine, personalized medicine in that kind of a setting.
Kennedy: It’s going to kill people to have their medical records as it relates to addiction kept separately from the rest of their medical records. Otherwise, what’s going to end up happening … is people are going to keep getting prescribed medication that is counter to what their real disease state is, which is addiction.
Q: You often hear about plans denying mental health treatment because they say it isn’t medically necessary. Is that dynamic something you are concerned about in terms of crafting an effective opioid addiction response?
Gingrich: We’ve been talking about opioids. Let me just talk about mental health. If you have depression, you are dramatically more likely to be sick. Now to say you don’t need to treat depression because it’s not a medical reality — when in fact it clearly affects your interaction with the entire world around you — is just frankly reactionary.
Reintegrating the brain into the rest of the body is absolutely essential to having the kind of long-term health and substantially lower cost [of care] than if you’re going to treat them separately. That’s a hangover from an earlier period.
The kind of MRIs that allow you to scan a living brain are about 20 to 25 years old. For most of the rise of modern medicine, the brain was a really unknown zone and was all based in guesswork. Well, that’s all changing. And the opioid recovery is a very good example of the scale of change we’re seeing.
Q: There is widespread interest in addressing opioid abuse. What can we reasonably expect? What policy action should happen immediately? And what might we see down the road?
Kennedy: It’s going to take reform on many different stakeholders’ parts. Obviously, there need to be changes made within the provider community, within the insurer community and within the advocacy community.
This is not a one-and-done — with a piece of legislation on the Hill, though, this is going to be an important period with respect to congressional action.
We intend to use our respective positions to inform our political party platforms, because the next Congress and the next president are going to need to have a new approach embedded into their policymaking.
This is not going to be done with this Congress. It’s going to be continually worked on in the years ahead.