[UPDATED on June 19]
The latest miracle machine in modern medicine — whose use has skyrocketed in recent years — is saving people from the brink of death: adults whose lungs have been ravaged by the flu; a trucker who was trapped underwater in a crash; a man whose heart had stopped working for an astonishing seven hours.
But for each adult saved by this machine — dubbed ECMO, for extracorporeal membrane oxygenation — another adult hooked up to the equipment dies in the hospital. For those patients, the intervention is a very expensive, labor-intensive and unsuccessful effort to cheat death.
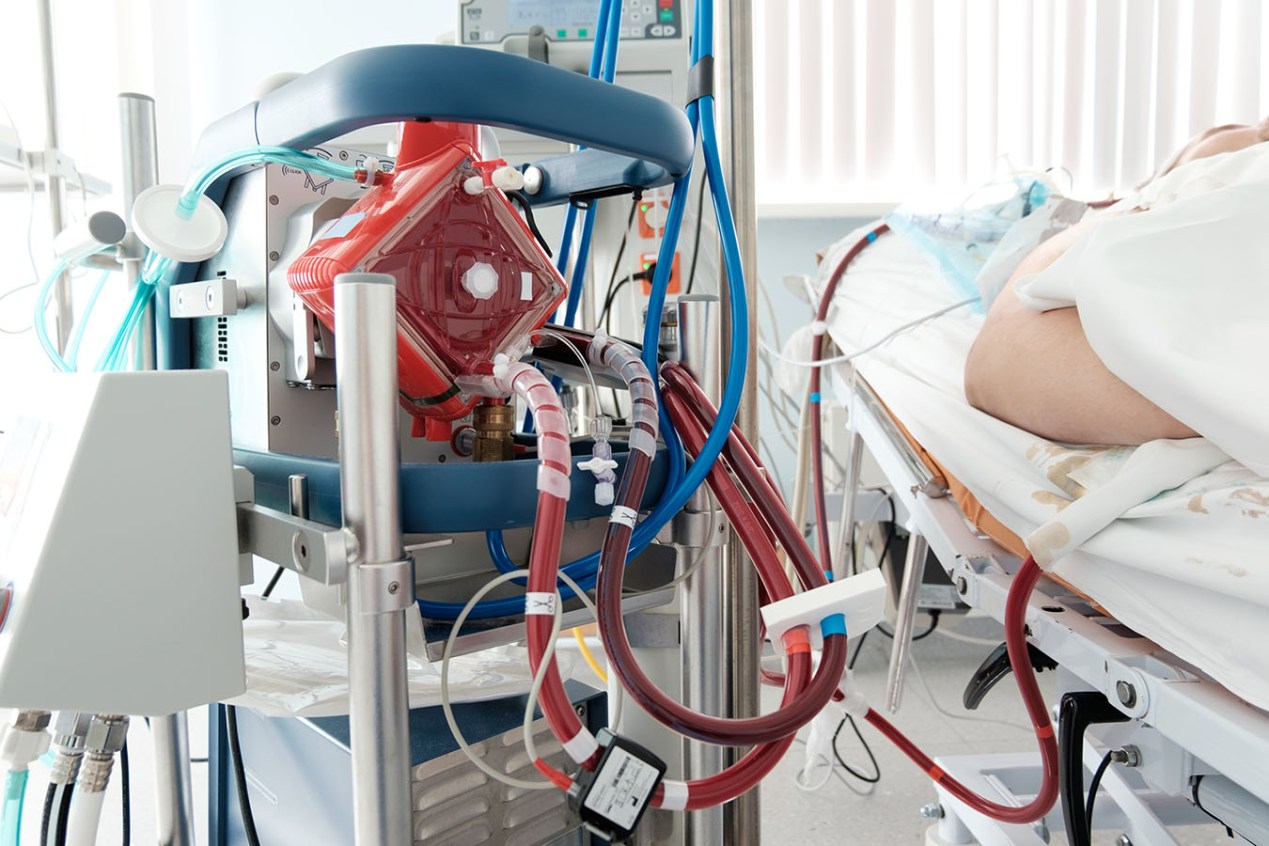
ECMO, the most aggressive form of life support available, pumps blood out of the body, oxygenates it and returns it to the body, keeping a person alive for days, weeks or months, even when their heart or lungs don’t work.
The invention is creating “an entirely new paradigm,” said Dr. Kenneth Prager, director of clinical ethics at Columbia University Irving Medical Center. “You have a heart that’s not working, yet the patient is not dead.”
Most commonly used for newborns, ECMO use has been growing dramatically among adults. In the United States, procedures tripled from 2008 to 2014, up to an estimated 6,890, according to the federal Agency for Healthcare Research and Quality.
Experts caution that as ECMO becomes more available, it is also being used as a last-ditch attempt to buy more time for dying patients with poor chances of survival.
ECMO is not designed to be a destination, but a bridge to somewhere — recovery, transplantation or an implanted heart device. But when patients are too sick to reach those goals, ECMO can become a “bridge to nowhere,” leaving the patient in limbo, possibly even awake and alert, but with no chance of survival outside the intensive care unit. Medical teams and families can be fiercely divided over when to pull the plug.
ECMO is very expensive, mostly due to the labor involved: A person on ECMO cannot live outside the ICU and must be continuously monitored for complications, such as blood clots, bleeding, infection and loss of blood to the limbs. Median charges for ECMO in 2014 were $550,000, making it the 15th-most-costly procedure that year, according to the AHRQ.
In one recent case, a teaching hospital charged $4.2 million for a 60-day ECMO stay for a 19-year-old man with acute respiratory distress syndrome who was comatose the entire time and did not survive, according to Dr. Merrit Quarum, CEO and founder of WellRithms, a cost-containment company. Quarum said a self-insured health plan is covering the bill.
The number of U.S. hospitals offering ECMO has more than doubled from 108 in 2008 to 264 today, according to a registry run by the Extracorporeal Life Support Organization (ELSO), which tracks most but not all programs.
“In the United States, the competition between hospitals is so intense that every hospital wants the ability to provide this level of care,” said Randy Bartilson, president of the ECMO Advantage consulting firm.
But “as ECMO expands, there’s still a lot of places that still don’t fully understand what it can do and how to use it,” he said.
Four patient stories highlight the promise — and complexities — of this game-changing technology.
The Seven-Hour Code
Dr. Jessica Zitter was working in the ICU in an Oakland, Calif., hospital one day when she got summoned for a code blue. A 60-year-old patient had arrived with a heart attack. His heart went into ventricular fibrillation, where it just wiggled like “a bag of worms,” she said.
Hospital staff started pumping their palms on the man’s chest and put a tube in his throat to help him breathe. Every so often, they stood back and zapped his heart with an electric shock. It didn’t work. So, they strapped onto his chest a LUCAS machine, which automatically performs chest compressions like a jackhammer.
The man’s oxygen levels were plummeting. At the same time, Zitter recalled, he kept moving, giving her the feeling there was a life to be saved. The medical team decided to go to the next level: ECMO. Everyone waited, with the jackhammering compressions still going, as an ECMO team scrambled to get there from another hospital across the city.
Zitter watched in awe as the ECMO team from the University of California-San Francisco got to work. They stuck one huge tube in a femoral artery and one in a femoral vein. As they pumped his blood out, it was black from deoxygenation. But after it ran through the ECMO machine, she recalled, it transformed into a bright red.
(Courtesy of University of Iowa Hospitals & Clinics)
Once on ECMO, the patient didn’t need his heart, so it could sit idle and recover. Zitter watched as oxygen returned to his body and brain. He was whisked back to UCSF.
Zitter, who has written about the overuse of modern technology to prolong death, wasn’t optimistic. The patient had coded, with people and machines ramming his failing heart, for an astonishing seven hours before ECMO arrived. But as she kept tabs on the patient, she was amazed to learn that he was able to recover and go home.
The case was a “big shocker,” Zitter said.
But it was “a crazy, crazy, crazy outlier case with a crazy, crazy, crazy outlier response,” she cautioned. “When these kinds of things happen, people tend to look at them and assume that they will have the same odds. The reality is that they won’t.”
When patients receive ECPR (ECMO for cardiopulmonary resuscitation), only 29% make it out of the hospital alive, according to international statistics from ELSO. Survival rates are higher for people who use ECMO for only the lungs (59%) or only the heart (42%), according to ELSO.
Saving ‘Santa’
A more common outcome for ECPR looks something like what Dr. Haider Warraich of Duke University Medical Center came across three or four years ago during his cardiology training.
Warraich was called to the waiting area of a lung transplant clinic, where a man in his 60s had collapsed on the floor due to a heart attack. The man, who had white hair and a scraggly beard, played Santa every Christmas, Warraich later learned. “Santa” — as Warraich refers to him in his upcoming book, “State of the Heart” — had received a new set of lungs after his were wrecked by smoking and lung disease.
The man’s heart, starved of oxygen, sped up into a malignant rhythm. CPR and electric shocks didn’t bring it back. Motivated to save not only the patient but the new set of lungs he had received, the team called in ECMO.
The ECMO squad arrived with catheters “the size of small javelins,” Warraich recalled. Once Santa was hooked up on ECMO, the exhausted CPR team could stop. Cardiologists did surgery on a blocked artery, but they never got his heart back to normal. The man lingered for a month, using ECMO for his heart, a ventilator for his lungs and dialysis for his kidneys, before he died.
In this case, using ECMO felt appropriate, Warraich said. But he said doctors need more guidance to determine which patients would benefit the most and to prevent overuse.
“If you have someone who is dying in front of you, it’s really hard to step back and think about it,” he said.
The technology, developed in the 1970s, was initially used primarily for newborns. Early clinical trials in adults were discouraging. But in 2009, the CESAR trial in the United Kingdom showed positive results for ECMO in adults with severe respiratory failure. Those findings, combined with improved technology and an epidemic of swine flu, prompted a swift growth of ECMO among adults. The average age for U.S. adults receiving ECMO is 51, one study found. About 1 in 10 ECMO cases are for people over 65.
Warraich and other experts say they are now concerned that new organ-donation rules may inadvertently spur hospitals to place more patients on ECMO: Under guidelines approved by the Organ Procurement and Transplantation Network last October, patients on ECMO jump to the front of the heart transplant waiting list.
An ‘Unbearable’ Choice
Once a patient is on ECMO, deciding when to stop can cause moral distress and division among medical staff, said Dr. Robert Truog, director of the Center for Bioethics at Harvard Medical School.
In one case Truog described in The Lancet, a 17-year-old boy came to the ICU at Boston Children’s Hospital, where Truog works as a physician. The boy, who had already had one lung transplantation for cystic fibrosis, was now in end-stage respiratory failure. The only way to save his life was to give him another set of lungs. He started on ECMO as a bridge therapy while he awaited transplantation.
The boy was fully conscious, doing homework, texting friends and visiting with family. But after two months of living in the ICU, he was diagnosed with untreatable cancer that made him ineligible to receive new lungs.
Clinicians were deeply divided over what to do next, Truog said. Some wanted to stop ECMO immediately because its original goal — a bridge to transplantation — was no longer possible.
Others argued that even though he couldn’t survive outside the ICU, the boy seemed to have a good quality of life on ECMO, and his family and friends “derived benefits from his continued survival,” Truog wrote. They argued that the family should have the right to continue this form of life support, just as with dialysis, ventilation or an artificial heart.
A third argument arose, Truog said: If leaving this patient on ECMO was appropriate, then in fairness “why don’t we put everyone with respiratory failure on ECMO?”
For the parents, Truog said, it was “unbearable” to choose a day or moment to turn off ECMO, because they knew their child would immediately die.
Clinicians devised an alternative the family would agree to: They decided not to replace the ECMO oxygenator, a part that needs to be changed every week or two when it develops blood clots. After about a week, the oxygenator gradually failed and the patient lost consciousness and died, Truog said.
The solution “allowed him to die in a way where we didn’t feel like we were choosing the moment of his death,” he said.
The solution was not optimal, Truog said. But “no matter how you do this, it’s going to be very emotionally upsetting to everyone. These are the cases that make some people leave the profession because they’re so hard.”
A Long Goodbye
Karen Ayoub had never heard of ECMO until her husband became direly ill.
Philip Ayoub, 58, an accountant and former comptroller for the National Football League, was a “huge personality” and a family man; the couple raised twin boys in Greenwich, Conn. Heart disease, which ran in his family, hit him early: He had his first coronary bypass surgery at age 30 and his second at 43, she said.
“He knew that his life might be foreshortened” and “tried to pack as much living into it as possible,” said Karen Ayoub, 55. Her husband told her he didn’t want any extraordinary lifesaving measures — he was happy with the life he had lived, she said.
In December 2017, he had a third bypass surgery at a hospital on Long Island, and it didn’t go well. His heart was weaker than anticipated. He became unconscious, and it wasn’t clear if he would ever wake up. He was transferred to Columbia University Irving Medical Center, which has an ECMO program.
Philip Ayoub, 58, an accountant and former comptroller for the National Football League, with his twin sons. Heart disease, which ran in his family, hit him early: He had his first coronary bypass surgery at age 30 and his second at 43.(Courtesy of Karen Ayoub)
Karen Ayoub said it was a fairly easy decision to put her husband on ECMO: “I thought he deserved any chance possible to recover,” she said. But she didn’t know how he’d react.
“I wasn’t sure if he was going to wake up and say, ‘Why did you do this? I didn’t want any of this!’” she recalled.
When her husband regained consciousness, he mouthed the words: “Why am I here?”
He remained in the ICU for two months, on a feeding tube, breathing tube, ECMO and dialysis. His time there was not easy, she said: Her husband, who had endured a series of mini-strokes during the bypass surgery, began to experience post-traumatic stress disorder, night terrors and side effects from medications.
The only option for further treatment, she said, was to get an implanted device that would help his heart pump. But as he weighed that decision, and the quality of life he would have, the window of time closed when he was eligible for the device, Karen Ayoub said.
When further treatment became out of reach, it was clear her husband was going to die.
“His body was failing him,” Karen Ayoub said. “It was time.”
She said the two months in the ICU felt like “a gift,” because she and her children got to spend extra time with her husband.
“I’ll always love you, I’ll always be with you,” he told his wife over and over during that time.
She said she would make the same choice again to initiate ECMO, but “I don’t know about him — he was the one laying in that bed for two months, being tortured by needles and night visions.”
After they ran out of treatment options, the family gave permission for the hospital to discontinue life support. Philip wasn’t afraid, she said: As his final day approached, he told her, “I can’t wait to see what comes next.”
Philip was sedated before ECMO was turned off. Karen Ayoub laid her head on her husband’s chest and held his hands as he died.
“It was peaceful and respectful,” she said, “exactly what he wanted.”
‘Futile’ Care
While the Ayoub family bravely accepted their fate, other families can’t bring themselves to let go, said Dr. Shunichi Nakagawa, a palliative care doctor at Columbia who cared for Philip Ayoub.
Some ECMO patients have severe, irreversible brain damage, can’t participate in decision-making and bear no chance of making it out of the hospital alive. For them, ECMO represents “the most extreme form of medical futility,” Nakagawa argued in an article he and Prager co-authored with a colleague in the journal Circulation. They argue that given the significant number of patients on ECMO who cannot survive, this “should prompt a societal discussion about current legal constraints on physicians” in discontinuing “new and powerful forms of life support.”
Whether they can stop ECMO depends on where they practice: Laws in states such as Idaho, Oklahoma and New York make it difficult to withdraw life-sustaining treatment like ECMO without consent from patients or their families, said Thaddeus Mason Pope, director of the Health Law Institute at Mitchell Hamline School of Law in St. Paul, Minn. But in states like California, Texas and Virginia, clinicians may withdraw ECMO without consent, he said.
Dr. Robert Bartlett, a pioneer of the ECMO field and professor emeritus at the University of Michigan, said he trains doctors that once ECMO becomes a bridge to nowhere, they should tell the family, “We talked about futility, and now we’re there. So we’re going to turn the circuit off tomorrow.”
“It’s extremely discourteous to the family to ask the family what to do,” he said.
At Cedars-Sinai Medical Center in Los Angeles — where patients with poor chances of survival were being put on ECMO, and families were getting conflicting messages about the potential benefit — staff launched an improvement effort that has created more consensus and consistency around appropriate ECMO care, according to Dr. Michael Nurok, medical director of the cardiac surgery ICU.
At the University of Southern California’s Keck Hospital, every family of an ECMO patient meets weekly with palliative care and other clinicians to talk about goals of care — conversations that have been “transformative” for families, said Dr. Sunita Puri, medical director of palliative medicine and supportive care.
In Boston, Dr. Daniela Lamas, a critical care doctor at Brigham and Women’s Hospital, said she has seen ECMO’s promise and its limitations.
“With every escalation and fancy machine comes a lot of hope,” Lamas said. “It’s really hard to temper that hope with the realities that with each new thing comes a host of ethical questions and dilemmas.”
ECMO, she said, is “a fantastic example of ‘just because you can, doesn’t mean you should.’”