Say you’re a rural Midwestern farmer in bed recovering from a major illness at your local hospital. It’s time for nurse’s check in, but there’s no knock on the door.
At Mercy Hospital in St. Louis, just over the foot of the bed, a camera whirls around and a monitor lights up to show a smiling face with a headset on.
“Good afternoon, this is Jeff with SafeWatch. Just doing my afternoon rounds,” he said in this training exercise.
Watching the video nurses in action, it’s a little hard to shake the Jetsons vibe, but this kind of health care is already alive and growing. On October 6, Mercy Hospital will open a new telemedicine mothership that will treat thousands of patients in 5 states.
The new facility will provide even more patients in remote parts of the Midwest and South with health monitoring that is comparable to what you could get in a big hospital, said Tom Hale, the executive medical director of Mercy Virtual.
“You can monitor their heart, their blood pressure, their respiratory rate, their temperature on a 24/7 basis,” he said. “You can monitor their position, so you can tell if they’ve been out of bed. You can tell if they’ve turned in bed.”
He said telemedicine can be high quality and cheaper than in-person care. A lot of what Hale and his team now provide is care for patients in rural areas, but its use may soon explode with a different group of patients: baby boomers who want to age at home instead of in a nursing facility. Industry analyst Sarah Turk of IBISWorld says that could propel telehealth to a $3.5 billion industry by 2020.
“Coverage will be expanded to include more physicians and more specialties and also a range of communications,” she said. “So instead of it being only interactive video consultation, it could be text messaging as well.”
But she said the telehealth boom still faces some big challenges. Many insurance companies have been slow to pay for telemedicine. Medicare, the healthcare coverage for Americans over 65, is a financial powerhouse and insurance companies often follow its lead on payments. Medicare only pays for telemedicine in rural or medically underserved areas and only when video conferencing is used.
But telemedicine has broadened as technology has developed. Now it could, for instance, use a smartphone app to monitor falls in the home, so insurance companies and Medicare have to re-think their payment criteria.
But Dr. Ashish Jha of Harvard University said insurers have good reason to be skeptical.
“If telemedicine really saved money, payers would be falling over themselves paying for this stuff, right? Because it would actually benefit their bottom line,” he says.
He says telemedicine does seem to provide good access to high quality medical care, but even though it could save money theoretically, that’s not what’s happening.
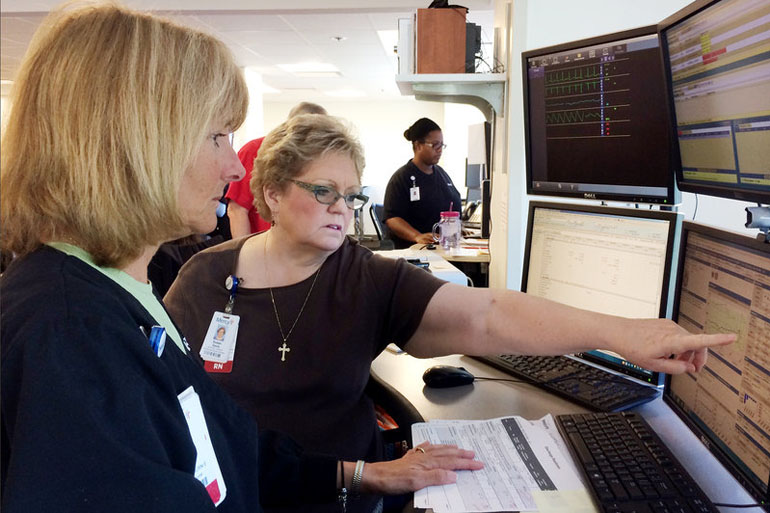
Mercy Virtual, based in St. Louis, will use video monitors like this to beam nurses into patients rooms in five states. (Photo by Alex Smith/KCUR)
“What tends to happen is that it tends to be an addition,” he explained. “You do the telemedicine, it leads to more tests. It leads to more follow-up visits. And over time, when you look at the data, it turns out that telemedicine overall is not necessarily a big cost saver.”
Still, Mercy Hospital is betting that expanding will be a good deal. With its new facility, the hospital can monitor nearly 7,500 acute care beds in five states, and they plan to expand from there.
This story is part of a reporting partnership with NPR, KCUR and Kaiser Health News.