JOHNSON CITY, Tenn. — Five years ago, rival hospital companies in this blue-collar corner of Appalachia made a deal. If state lawmakers let them merge, leaving no competitors, the hospitals promised not to gouge prices or cut corners. They agreed to dozens of quality-of-care conditions, spelled out with benchmarks, and to provide hundreds of millions of dollars in charity care to patients in need.
Today, Ballad Health’s 20 hospitals remain the only option for hospital care for most of about 1.1 million residents in a 29-county region at the nexus of Tennessee, Virginia, Kentucky, and North Carolina. But Ballad has not met many of the quality benchmarks nor provided much of the charity, spurring discontent among those with no choice but to rely on Ballad for their care.
Two dozen states, from Florida to Washington, have at some point passed so-called COPA laws that allow hospital systems to merge into monopolies, disregarding warnings from the Federal Trade Commission that such mergers can become difficult to control and may decrease the overall quality of care. In the case of Ballad, the nation’s largest-known COPA deal, public records suggest that is exactly what happened.
Documents released by the Tennessee Department of Health show:
- Ballad has not fulfilled the annual charity care obligation it made to Tennessee, falling short by about $148 million over a four-year span. In those same years, Ballad took thousands of patients to court to collect unpaid bills.
- Ballad failed to meet about 80% of benchmarks designed to monitor and improve its quality of care — including rates of infection and death — in the most recent year for which data is available. Federal health officials cited some of these same problems this year in issuing one-star ratings to three Ballad hospitals, including a flagship, Johnson City Medical Center.
“The state of Virginia and the state of Tennessee took a chance on [Ballad] to do the right thing,” said Michele Johnson, executive director of the Tennessee Justice Center, a nonprofit focused on health care for the poor. “And they’ve proven that they are not worthy of that chance.”
In a two-hour interview with KFF Health News, Ballad Health CEO Alan Levine defended the merger as “hugely successful” for a region rife with poverty and sickness, saying his company had planted seeds of better health that “you can’t quantify today.” More specifically, Levine said the enormous pressure of the coronavirus pandemic caused Ballad’s slumping quality of care. He attributed charity care shortfalls to Medicaid changes beyond Ballad’s control and new preventive care programs that keep patients out of the hospital so they don’t need charity.
Levine said the Ballad merger had likely prevented at least three hospital closures and kept giant corporations from swooping into Appalachia to buy up the scraps.
“Our critics say, ‘No Ballad. We don’t want Ballad.’ Well, then what?” Levine said. “Because the hospitals were on their way to being closed.”
Ballad is centered in Tennessee and Virginia’s Tri-Cities region, a cluster of hardscrabble towns and wooded foothills that is home to the famous Bristol Motor Speedway and recognized by Congress as “the birthplace of Country Music.” Census data shows the Tri-Cities poverty rate is about 30% higher than the national average, and residents’ general health is below average for the nation and their respective states, according to the BlueCross BlueShield National Health Index.
Ballad launched in 2018 after state officials approved the nation’s largest-known Certificate of Public Advantage, or COPA, agreement, which waived anti-monopoly laws so the region’s only two hospital systems — Mountain States Health Alliance and Wellmont Health System — could merge. To offset the perils of a monopoly, the COPA requires Ballad to agree to increased oversight by the state and a long list of special conditions, including limiting price increases, maintaining quality, and providing charity care. Ballad also committed to investing $308 million over 10 years to improve the health of the region, some of which it has spent on a low-to-no-cost care network for the uninsured and expanded addiction treatment services.
Even with this spending, Ballad has turned a profit. The company generated net income of more than $143 million and $63 million in fiscal years 2022 and 2021, respectively, while receiving $175 million in pandemic relief funds, according to an S&P Global Ratings independent analysis, which excludes items like gains and losses separate from hospital operations.
The merger was profitable for Levine too. His total compensation has nearly doubled to about $4.3 million since the merger, including some deferred retirement payments, according to reports filed with the IRS. Prior to Ballad, Levine worked as a high-level health official in Florida and Louisiana and was an executive at two larger hospital corporations, HCA Healthcare and Health Management Associates. Federal prosecutors accused both companies of widespread health care fraud during some of the years when Levine was one of their leaders, claims the companies denied but later paid hundreds of millions of dollars to settle.
Nationwide, the COPA model is uncommon but gaining momentum. COPAs have been used in about 10 hospital mergers over the past three decades, including two in Texas and one in Louisiana in just the past three years, and another is being proposed in Indiana. Nineteen states have laws on the books allowing for COPAs, although not all have approved a specific merger, and five other states passed COPA laws and later repealed them, according to The Source on HealthCare Price & Competition, a website by the University of California College of the Law-San Francisco.
Rahul Rao, a deputy director of the Bureau of Competition at the Federal Trade Commission, which consistently opposes COPAs, said removing hospital competition leads to predictable results — rising prices, decreasing quality, and monopolies that are very hard to break up.
Rao said the FTC has for years studied how the Ballad merger is affecting health care in the region but that it is not yet ready to publish its findings.
“States should be very wary and distrustful of COPAs in general,” Rao said. “It’s very hard to unscramble the eggs.”
Tennessee began to pave the way for Ballad in 2015 when state Sen. Rusty Crowe (R-Johnson City) co-sponsored a bill allowing for the merger, which was later mirrored in Virginia. Crowe was also working as a contractor for Mountain States Health Alliance when the bill was introduced, and since the merger he has been similarly contracted with Ballad, the lawmaker said.
Tennessee financial disclosure records confirm Crowe was paid by both hospital systems but don’t say how much or for what. Crowe, who did not agree to an interview, said in an email that he was hired to “help in the development of wound care and hyperbaric medicine” and that he “complied with all the Senate ethics code requirements regarding any potential conflict of interest.”
Tennessee and Virginia health officials have concluded annually that the merger remains beneficial to the public and, in reports and interviews, credited Ballad for weathering the pandemic and keeping hospitals open.
Dennis Barry, one of the state monitors hired to keep tabs on Ballad, said he believed Ballad had largely lived up to the agreement, or at least the “intent.” Barry dismissed the FTC’s position that hospital competition is necessarily beneficial and said no one knows how the region would have fared without the merger.
“In a sense, we’ll never be able to determine whether or not this was a good idea or a bad idea,” Barry said. “I view it as an experiment.”
As Ballad fell short of its COPA benchmarks, state officials took steps to relax the oversight of its hospitals, particularly in Tennessee. Both Tennessee and Virginia gave Ballad more time to spend tens of millions to benefit the region, and Tennessee officials have repeatedly waived Ballad’s annual charity care obligation. Tennessee in 2021 stopped publishing a “final score” for Ballad’s adherence to the COPA terms and in 2022 revised COPA rules so Ballad could oppose the opening of competing hospitals or other medical facilities in the region, according to state documents. A local COPA advisory council, created to hear complaints from residents, no longer hosts public hearings.
Ballad Cites Pandemic Amid Quality Decline
Ballad has failed to meet quality-of-care benchmarks established in the COPA agreement in recent years, according to public reports from the Tennessee government and the hospital system itself. For example, a Tennessee report shows that from July 2021 through June 2022, Ballad hospitals fell short of 61 of 75 benchmarks, including some about sepsis, surgery-related infections, emergency room speed, and rates of readmission and death from heart failure.
The Centers for Medicare & Medicaid Services this year issued one-star ratings to three Ballad hospitals, all of which had ratings of at least two stars before the merger. Because CMS calculates star ratings from data collected over several years, the ratings released this year are the first to grade the Ballad hospitals entirely on post-merger data.
Levine, citing arguments similar to those of other hospital leaders, insisted the CMS five-star rating system is broken because it judges hospitals on a sliver of patients and doesn’t account for poor health in the region. He said Ballad fell short of the COPA benchmarks because the coronavirus overwhelmed hospitals and sparked an unprecedented nursing turnover.
But Ballad’s hospitals have since rebounded, Levine said, pointing to partial data on the company website — not yet reported by the states — that appears to show improving performance as of this summer. And Levine said internal data showed Ballad was now tracking with the top 10% of U.S. hospitals on some quality-of-care metrics.
“We went way backwards during covid, no question about it. And now we’ve emerged out of covid,” Levine said. “We’re recovering faster than other people.”
Erik Bodin, a Virginia Department of Health official who oversees the agreement with Ballad, said the pandemic caused quality issues at hospitals across the state, including Ballad’s, which were “not acceptable” but “to some extent understandable.” Bodin said Virginia still has “concerns” and is “watching very closely” because not all of Ballad’s metrics are rebounding.
The Tennessee Department of Health, which has the most robust role in regulating Ballad, declined an interview request and did not answer questions submitted in writing.
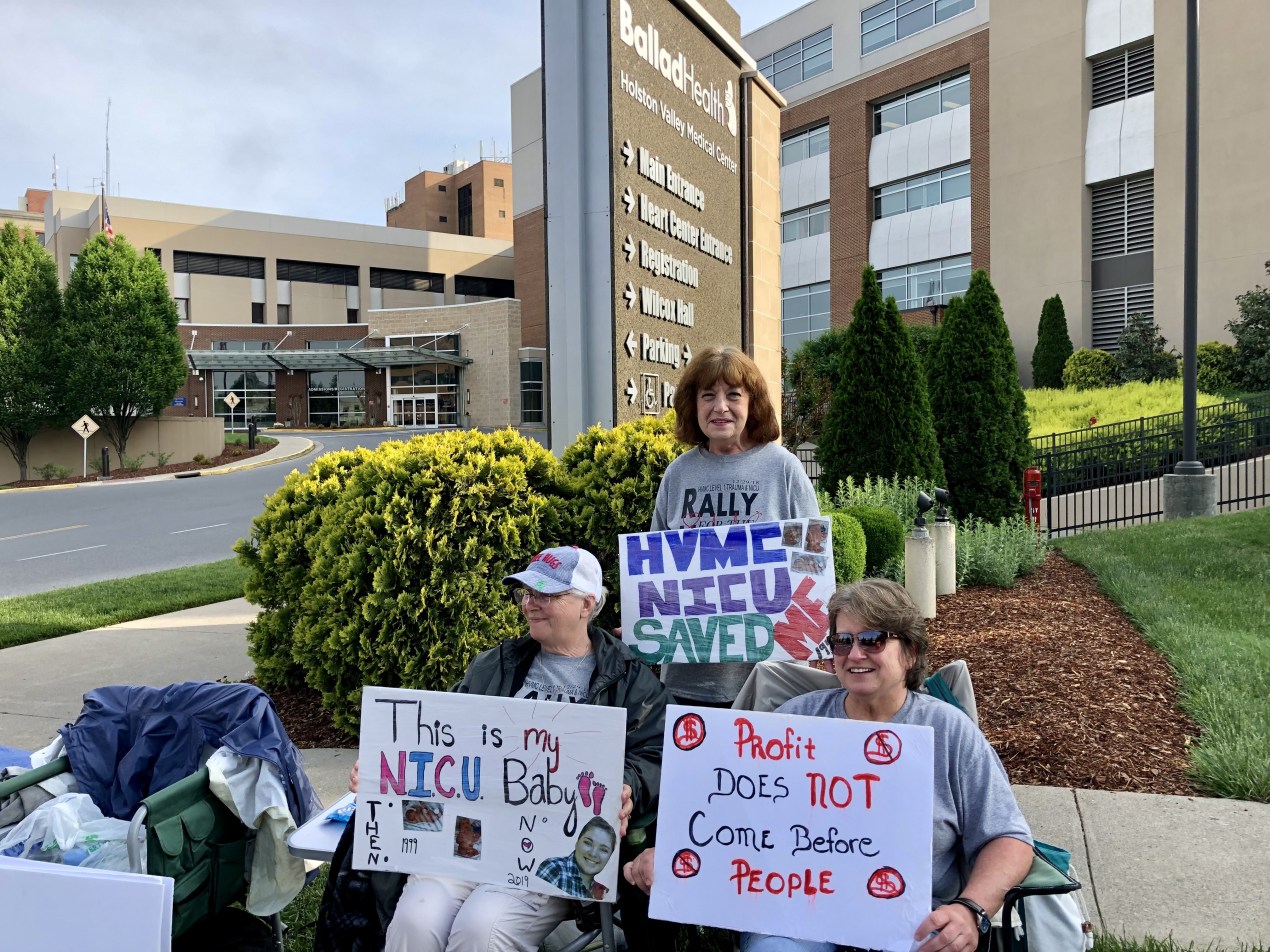
Ballad has also cut back on facilities for patients with life-threatening conditions. Citing redundancy with other hospitals, it downgraded the capabilities of trauma centers at Bristol Regional Medical Center and Holston Valley Medical Center and closed the intensive care unit at Sycamore Shoals Hospital. Ballad also shuttered the Holston Valley neonatal ICU. Residents were so angry that protesters gathered outside Holston Valley for eight months.
“I packed a sleeping bag, a backpack, and my laptop bag. I made two signs in my living room,” said Dani Cook, the protest leader and grandmother of a former Holston Valley NICU patient. “And next thing you know, 50 people showed up.”
One month after Holston Valley’s trauma center was downgraded, Jeremiah Shane Fields, 37, died at the hospital from chest injuries sustained in a car crash. According to a CMS investigation report obtained by KFF Health News, Fields’ blood pressure dropped for hours before his death, but his doctor did not come to his bedside as his condition deteriorated.
Holston Valley’s chief medical officer, who is quoted in the report but not named, called the case a “fundamental failure of basic trauma care” in which Fields’ doctor was “not following essential standards,” according to the report. Holston Valley was cited for “deficiencies” that were likely to harm patients, which the hospital immediately corrected, the report states.
Fields’ family has filed an ongoing lawsuit alleging negligent care, and Ballad Health has denied all wrongdoing in court filings. Molly Luton, a spokesperson for Ballad, said that Fields’ death was “an outlier” and “not the result of a systemic issue.”
Fields’ mother, Penny Meade, 59, said she believed the hospital could have done more to save her son.
“It used to be wonderful,” Meade said. “But then everything changed. They took it all away, after that merger.”
‘Helping People’ vs. ‘Coming After Them’
Ballad has fallen short of the annual charity care commitment in the COPA agreement by about $20 million to $48 million each year, according to Tennessee Department of Health documents. The agency waived this obligation each year after it wasn’t met, the documents show.
Charity care comes in two forms: free or discounted care for low-income patients, or the amount left over when Medicaid patients are treated but their entire cost is not covered. Most of Ballad’s charity care is from the second scenario, the documents show.
Ballad said in its annual reports it is unable to meet its charity care obligation because after the COPA was negotiated both Tennessee and Virginia increased their Medicaid reimbursement and Virginia expanded Medicaid to cover more people, leaving fewer people uninsured and in need of charity. (Tennessee has not expanded Medicaid.)
Levine added that Ballad’s new Appalachian Highlands Care Network provides preventive care to uninsured residents.
“We are doing everything we can, for instance, to manage their diabetes so that they don’t end up with a spike and end up in the ER,” Levine said. “That reduces your charity care.”
Some are unconvinced. Chris Garmon, a former FTC economist and a leading expert on COPAs at the University of Missouri-Kansas City, said Ballad had put forth a “strange defense” for its lack of charity care in a state where so many are uninsured.
“Last time I checked, Tennessee had not expanded Medicaid,” Garmon said. “This sounds like Ballad is pushing the envelope, like a toddler, trying to see when their parents will actually institute some discipline.”
As it was falling short of its charity commitment, Ballad filed thousands of debt collection lawsuits against patients in its first two years of operation, according to reporting from The New York Times and Modern Healthcare.
Levine said that Ballad does not sue patients who qualify for charity care and that its lawsuits slowed significantly after it adopted a more generous charity care policy in 2020. Ballad now offers free care to those who live at or below 225% of the federal poverty level, or an income of less than $67,500 for a family of four.
But the company still takes many patients to court. For example, in Tennessee’s Sullivan County, one of the most populous areas in Ballad’s market, the company has filed about 500 lawsuits since enacting the new charity care policy, court records show.
Wendy McClanahan, 44, said Ballad started garnishing her paycheck this summer over a lingering debt from a 2017 surgery. McClanahan said she was unemployed and unable to afford the bill at the time and she believed it was written off until court papers arrived in the mail.
Ballad will take 25% of McClanahan’s paycheck until she has paid off $2,747, court records show. McClanahan said she’s working overtime at her office job to make up for the lost income.
“They’re supposed to be helping people instead of coming after them,” she said. “It’s a lot of money to me, you know, and nothing to them.”
KFF Health News correspondent Bram Sable-Smith contributed to this report.