When a rural community loses its hospital, health care becomes harder to come by in an instant. But a hospital closure also shocks a small town’s economy. It shuts down one of its largest employers. It scares off heavy industry that needs an emergency room nearby. And in one Tennessee town, a lost hospital means lost hope of attracting more retirees.
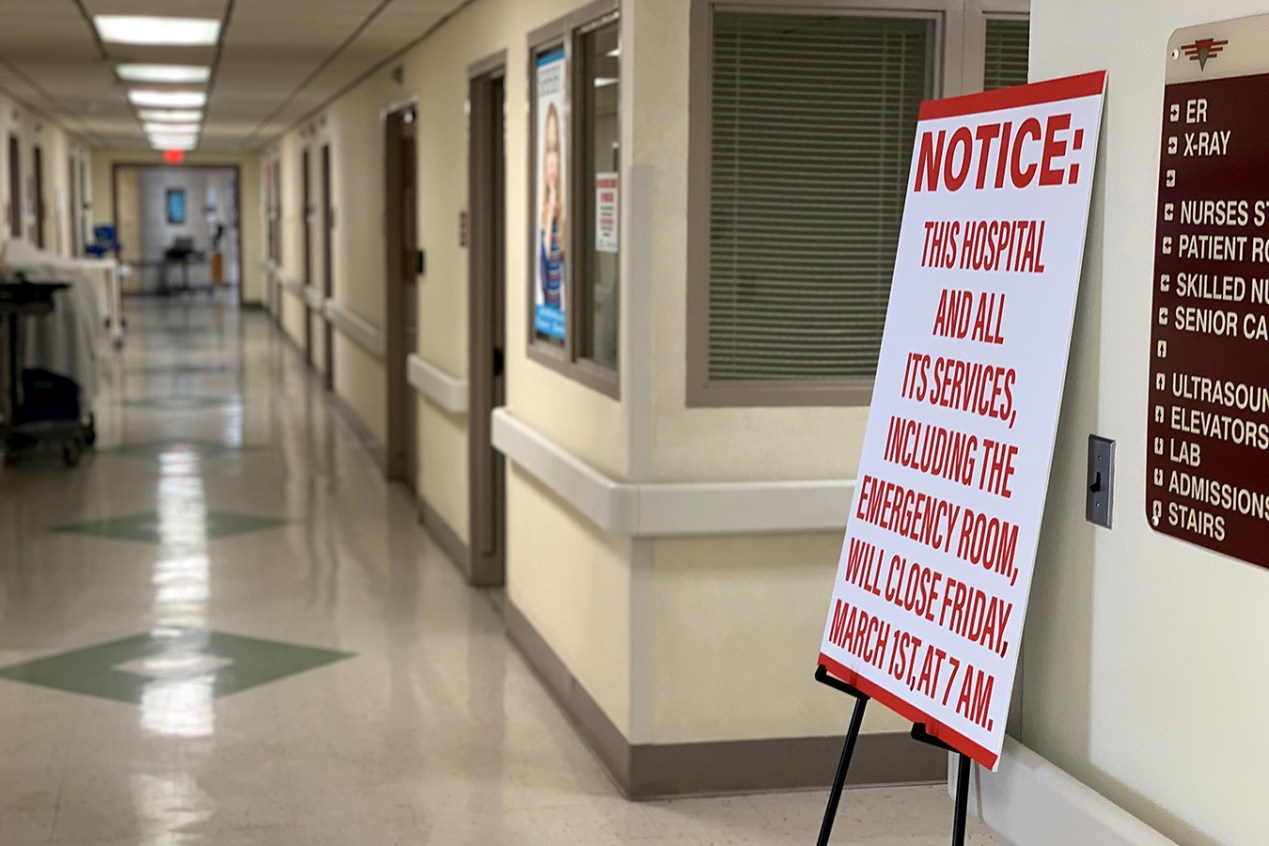
Seniors, and their retirement accounts, have been viewed as potential saviors for many rural economies trying to make up for lost jobs. But the epidemic of rural hospital closures is threatening those dreams in places like Celina, Tenn. The town of 1,500, whose 25-bed hospital closed March 1, has been trying to position itself as a retiree destination.
“I’d say, look elsewhere,” said Susan Scovel, a Seattle transplant who arrived with her husband in 2015.
Scovel’s despondence is especially noteworthy given she leads the local chamber of commerce effort to attract retirees like herself. She considers the wooded hills and secluded lake to hold scenic beauty comparable to the Washington coast — with dramatically lower costs of living; she and a small committee plan getaway weekends for prospects to visit.
When she first toured the region before moving in 2015, Scovel and her husband, who had Parkinson’s, made sure to scope out the hospital, on a hill overlooking the sleepy town square. And she has rushed to the hospital four times since he died in 2017.
“I have very high blood pressure, and they’re able to do the IVs to get it down,” Scovel said. “This is an anxiety thing since my husband died. So now — I don’t know.”
She can’t in good conscience advise a senior with health problems to come join her in Celina, she said.
Closure of the hospital meant 147 nurses, aides and clerical staff had to find new jobs. The hospital was the town’s second-largest employer, after the local school system.(Blake Farmer/WPLN)
When Seconds Count, Delays In Care
Celina’s Cumberland River Hospital had been on life support for years, operated by the city-owned medical center an hour away in Cookeville, which decided in late January to cut its losses after trying to find a buyer. Cookeville Regional Medical Center executives explain that the facility faced the grim reality for many rural providers.
“Unfortunately, many rural hospitals across the country are having a difficult time and facing the same challenges, like declining reimbursements and lower patient volumes, that Cumberland River Hospital has experienced,” CEO Paul Korth said in a written statement.
Celina became the 11th rural hospital in Tennessee to close in recent years — more than in any state but Texas. Both states have refused to expand Medicaid in a way that covers more of the working poor. Even some Republicans now say the decision to not expand Medicaid has added to the struggles of rural health care providers.
The closest hospital is now 18 miles away. That adds another 30 minutes through mountain roads for those who need an X-ray or bloodwork. For those in the back of an ambulance, that bit of time could mean the difference between life or death.
Staff members posted photos and other memorabilia in the halls — reminders of happier times — in the weeks before its closure.(Blake Farmer/WPLN)
“We have the capability of doing a lot of advanced life support, but we’re not a hospital,” said Natalie Boone, Clay County’s emergency management director.
The area is already limited in its ambulance service, with two of its four trucks out of service.
Once a crew is dispatched, Boone said, it’s committed to that call. Adding an hour to the turnaround time means someone else could likely call with an emergency and be told — essentially — to wait in line.
“What happens when you have that patient that doesn’t have that extra time?” Boone asked. “I can think of at least a minimum of two patients [in the last month] that did not have that time.”
Residents are bracing for cascading effects. Susan Bailey hasn’t retired yet, but she’s close. She has spent nearly 40 years as a registered nurse, including her early career at Cumberland River.
“People say, ‘You probably just need to move or find another place to go,’” she said.
Bailey and others are concerned that losing the hospital will soon mean losing the only three physicians in town. The doctors say they plan to keep their practices going, but for how long? And what about when they retire?
“That’s a big problem,” Bailey said. “The doctors aren’t going to want to come in and open an office and have to drive 20 or 30 minutes to see their patients every single day.”
Susan Bailey has lived most of her life in Celina and started her nursing career at Cumberland River Hospital. She now worries that its closure will drive away the town’s remaining physicians.(Blake Farmer/WPLN)
Closure of the hospital means 147 nurses, aides and clerical staff have to find new jobs. Some employees come to tears at the prospect of having to find work outside the county and are deeply sad that their hometown is losing one of its largest employers — second only to the local school system.
Dr. John McMichen is an emergency physician who would travel to Celina to work weekends at the ER and give the local doctors a break.
“I thought of Celina as maybe the ‘Andy Griffith Show’ of health care,” he said.
McMichen, who also worked at the now-shuttered Copper Basin Medical Center, on the other side of the state, said people at Cumberland River knew just about anyone who would walk through the door. That’s why it was attractive to retirees.
“It reminded me of a time long ago that has seemingly passed. I can’t say that it will ever come back,” he said. “I have hopes that there’s still some hope for small hospitals in that type of community. But I think the chances are becoming less of those community hospitals surviving.”
This story is part of a partnership that includes Nashville Public Radio, NPR and Kaiser Health News.