When Will Lightbourne looked at the statistics behind California’s coronavirus cases, the disparities were “blindingly clear”: Blacks and Latinos are dying at higher rates than most other Californians.
As of Monday, Latinos account for 45.6% of coronavirus deaths in a state where they make up 38.9% of the population, according to data collected by the California Department of Public Health. Blacks account for 8.5% of the deaths but make up 6% of the population.
Lightbourne, who led California’s Department of Social Services under Gov. Jerry Brown, describes this pandemic as one that “rips the bandage off” a health care system long riddled with inequity.
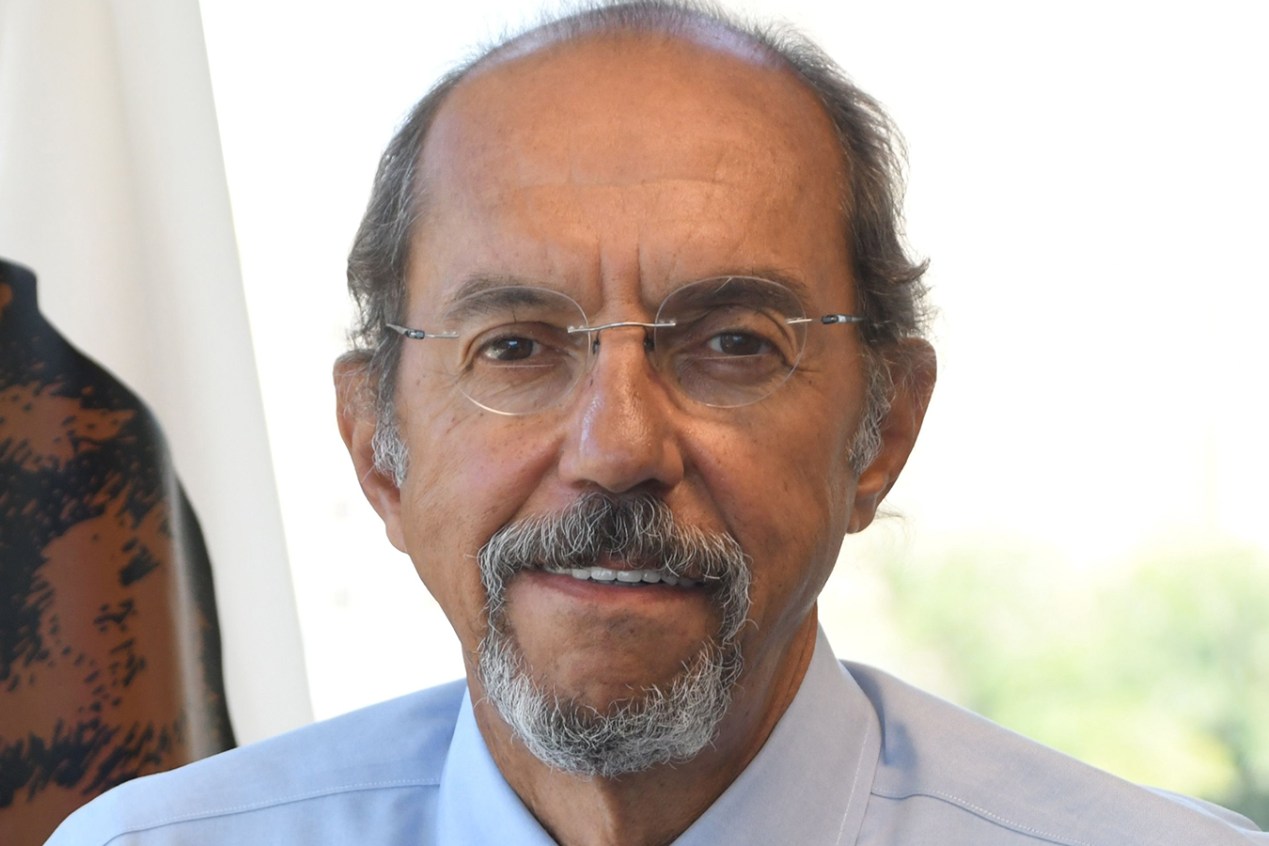
So, when Gov. Gavin Newsom asked Lightbourne, 70, to come out of retirement in June to lead the Department of Health Care Services, he said, he couldn’t say no.
“He has committed his whole professional life to public service,” said Mike Herald, director of policy advocacy at the Western Center on Law & Poverty. “He’s not joking when he talks about the importance of these issues and the important role that government plays in addressing societal inequities.”
The Department of Health Care Services oversees the state’s Medicaid program for low-income people, called Medi-Cal, which provides health care to some 12.5 million Californians.
Lightbourne said he sees the job as a chance to refocus Medi-Cal on reducing disparities — improving people’s health not only by providing better access to doctors, but also by linking them with behavioral health programs and using health care dollars to get them into housing.
He said the department also plans to amend contracts with health providers and use routine performance reviews to make sure providers are addressing disparities.
Health care advocates say Lightbourne has a track record of getting things done.
At the Department of Social Services, he persuaded Brown, a known penny pincher, to increase cash assistance to low-income families, restoring cuts lawmakers had made in the Great Recession. And he was instrumental behind the scenes in the repeal of the contentious policy that had prohibited Californians from receiving increased welfare income if they had more children while receiving public assistance, Herald said.
“Will is very purpose-driven and has made substantive changes in every role he has ever had,” said Graham Knaus, executive director of the California State Association of Counties.
Before embarking on state service, Lightbourne served as director of the Santa Clara County Social Services Agency, the Human Services Agency of the City & County of San Francisco and the Santa Cruz County Human Services Agency.
Lightbourne’s local and state experience give him a valuable skill set as state and county officials grapple with providing health care to some of California’s most vulnerable residents during a pandemic, Knaus and other advocates said.
The task won’t be easy. The previous director of the Department of Health Care Services, Brad Gilbert, left the job after less than four months.
Lightbourne talked to California Healthline about why he returned to state government, how the department is responding to COVID-19 and how he hopes to improve access to health care for those who need it. The interview has been edited for length and clarity.
Q: Why did you come out of retirement to take a job that’s difficult under normal circumstances — and even tougher during a pandemic?
Events of the past six months have made it blindingly clear that we’ve got structural inequities that are not just immoral but are, at an existential level, unsurvivable. It’s a pandemic that landed on top of a pandemic of inequalities, opportunity and income that’s been raging since the 1980s. And that pandemic has been enabled by a pandemic of racism that has rotted in our society for generations.
I think we have to use the moment to insist that our publicly financed health care system really partners up with our public health network and with our social safety-net system to address community and population health with a laser focus on reducing disparities.
Q: How has the department responded to COVID-19 to address the most vulnerable Californians?
The growth in telehealth is something that would not have occurred without this experience. There’s work still underway to look at how we can come up with some approaches to reduce the number of people in skilled nursing facilities, where the rate of spread is so much more severe and with really mortal results.
I have the suspicion that we’re never really going to get to a point where we say the effect of COVID is over. The mere fact that so much health care utilization is down now, particularly down in the places where people who start at a disadvantage normally seek care, we’re going to find long-term health consequences into the future, even post-vaccine.
Q: In January, Gov. Newsom outlined a proposal to broaden a Medi-Cal program known as CalAIM that addresses physical and behavioral health needs in patients’ care, and even pays for their housing with health care money. Can your department still move forward with those goals even though there isn’t money in the budget for it?
We may be delayed to some extent. It was never intended initially as a big-bang system change. It was always going to be a degree of iterative development, and that remains true — whether some things have to go a little slower because of money reasons.
Q: You have talked about access to health care and how COVID-19 has really highlighted systemic disparities. In Medi-Cal, lack of access to care has long been a problem, especially in rural areas. So has inadequate care for children. Are those issues you intend to address?
One of the things we need is an adequate network of providers that really covers the medically underserved areas of the state. We need to work effectively with our rural health clinics, as well as our urban Federally Qualified Health Centers to expand access, particularly to the populations that historically haven’t had that access.
In terms of services for children, that’s a big part of that agenda both in physical and behavioral health and also the dental health system. There’s a big focus on how to improve access and preventive services for children.
Q: In the Great Recession, California lawmakers made many deep cuts to safety-net programs, some of which have been restored only recently. The governor proposed a number of health care-related cuts this year that were ultimately rejected by the legislature. How will you ensure that Medi-Cal enrollees won’t see their benefits scaled back in the future?
It’s going to be my job to make the case not to reduce services that poor people rely on. That said, we live in the real world and if we ever have to reduce things, my approach would be to try to say, “How can we reduce things we can readily rebuild rather than destroy things that are foundational?”
Goal No. 1 at this point is to work very closely with our congressional delegation to really encourage the federal government to support the core services and activities so that we can meet the needs of the people of the state.
This story was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.