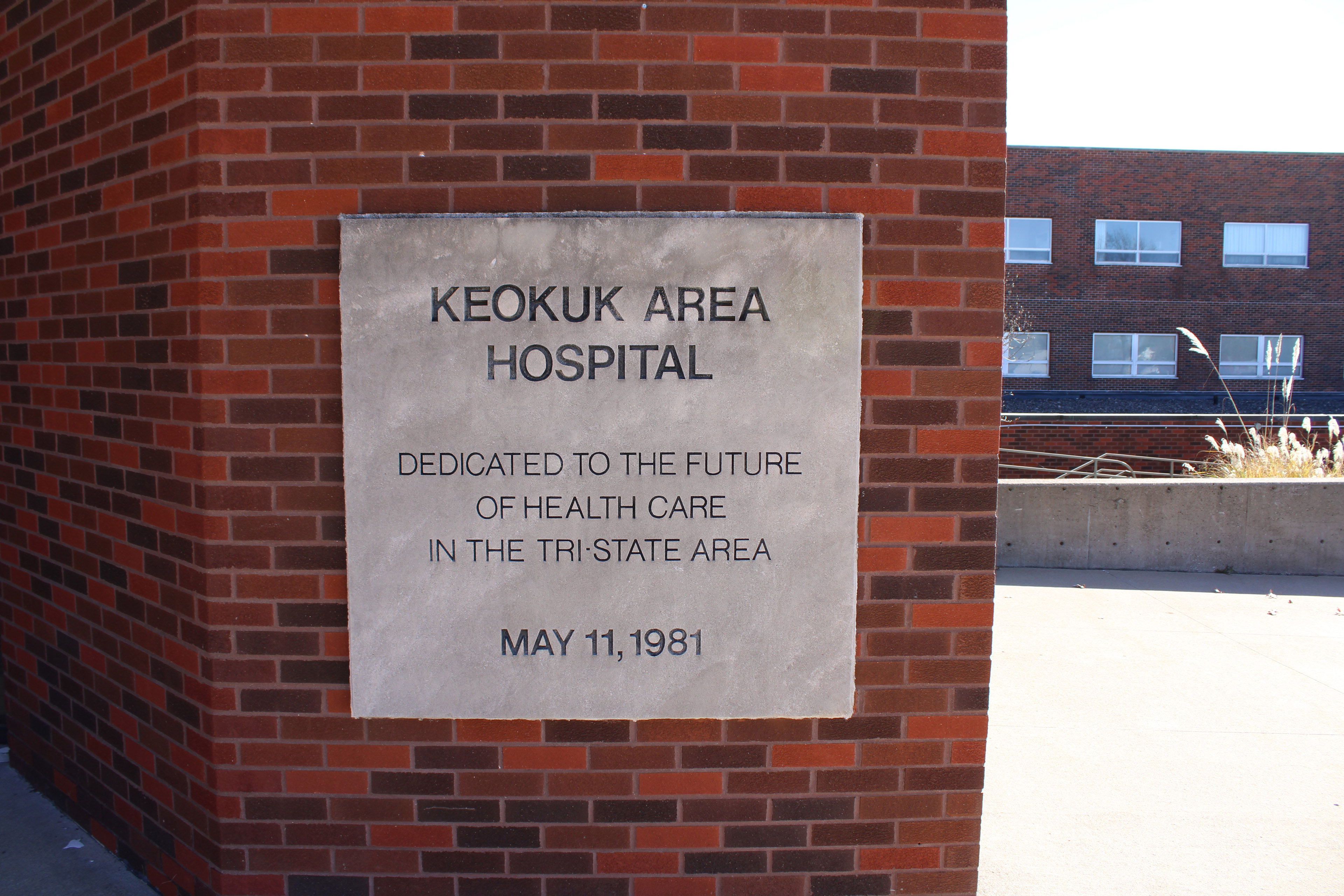
KEOKUK, Iowa — Folks in this Mississippi River town hope a new federal program can revive the optimism engraved long ago in a plaque on the side of their hospital.
“Dedicated to the Future of Health Care in the Tri-State Area,” the sign declares. “May 11, 1981.”
More recent placards posted at the facility’s entryways are ominous, however. “Closed,” they say. “No Trespassing.”
The Keokuk hospital, which served rural areas of Iowa, Illinois, and Missouri, closed in October 2022. But new owners plan to reopen the hospital with the help of a new federal payment system. The Rural Emergency Hospital program guarantees hospitals extra cash if they provide emergency and outpatient services but end inpatient care.
“We’ve been without a hospital for over a year — and I don’t think anybody in Keokuk or the surrounding areas will be picky in any way, shape, or form,” said Kathie Mahoney, mayor of the town of about 9,800 people. She said residents would prefer to have a full-service hospital with inpatient beds, even though those types of beds had been used sparingly in recent years.
The revival of the Keokuk hospital would mark a small victory in the nationwide struggle to save rural hospitals, which continue to close due to staffing shortages, low reimbursement rates, and declining patient numbers. The new federal program, which went into effect in January 2023, is meant to stem the closures. But there have been growing pains, said George Pink, deputy director of the North Carolina Rural Health Research Program, which tracks hospital closures and conversions.
Just 18 of the more than 1,700 eligible rural hospitals nationwide have applied for and won the new designation. Many hospitals are reluctant to give up inpatient services entirely, and some are concerned about how other payment streams could be affected, rural health leaders say. The new designation’s unclear definition of “rural” has also caused confusion.
“We are still in an era of rural hospital closures,” Pink said. Nine hospitals closed in 2023, and that number could rise in 2024, he said. An influx of federal relief funds during the pandemic kept struggling hospitals afloat, but now that money is largely gone.
The Rural Emergency Hospital program is the first new federal payment model for hospitals since 1997. Dora Hughes, acting chief medical officer of the Centers for Medicare & Medicaid Services, said the new model’s criteria are outlined by statute and “hospitals should consider specific circumstances before making the decision to apply.”
The federal agency is providing outreach to rural communities and welcomes feedback, Hughes wrote in an email to KFF Health News.
Now, rural health leaders and federal lawmakers are working quickly to tweak the new program to attract more applicants, said Carrie Cochran-McClain, chief policy officer of the National Rural Health Association.
Currently, facilities that convert to rural emergency hospitals receive a 5% increase in Medicare payments, plus an average annual payment of about $3.2 million, in exchange for giving up their expensive inpatient beds and focusing solely on emergency and outpatient care. Rural hospitals with no more than 50 beds, like Keokuk’s, that closed after the law was signed on Dec. 27, 2020, are eligible to apply for the program and reopen with emergency and outpatient services.
More than 100 rural hospitals nationwide have inquired about converting, said Janice Walters, interim executive director for the Rural Health Redesign Center, which has a federal grant to provide technical assistance to hospitals that want to apply.
But only about a quarter of those inquiries are likely to become a rural emergency hospital, and persuading more troubled hospitals to make the leap would require regulators to make changes, Walters said.
Her advice? “Give them 10 beds to just take care of their community.”
In a journal article published last year, general surgeon Sara Schaefer worried about the unintended consequences of getting rid of rural inpatient beds. Schaefer, who spent six months of medical school at a small rural Idaho hospital, said she saw firsthand how difficult it was for the hospital to transfer patients to bigger facilities, which were often too full to take them.
“There has to be a better way,” said Schaefer, who is also a research fellow at the Center for Healthcare Outcomes & Policy at the University of Michigan.
The rural health association’s Cochran-McClain said lawmakers are considering changes that could allow the hospitals to:
- Keep overnight beds for patients who need moderate levels of care, such as those with pneumonia or in need of physical therapy after surgery.
- Allow participation in a federal drug discount program called 340B, which provides hospitals with extra revenue.
- Keep inpatient psychiatric or rehabilitation units open.
- Clarify eligibility, including which facilities qualify under the definition of “rural” and whether the hospitals that closed before the 2020 date in the law can apply.
Updates to the law could affect communities nationwide. In Fort Scott, Kansas, where the hospital closed in late 2018, Mayor Matthew Wells said the community wants the eligibility date pushed back. U.S. Sen. Jerry Moran (R-Kan.) introduced a bill in December that, if passed, would push eligibility back to 2015.
“This is a matter of life and death to my community,” Wells said. “I see a clear path, but the federal regulations in particular make that path nearly impossible.”
In Holly Springs, Mississippi, hospital chief executive Kenneth Williams said he doesn’t understand the federal definition of “rural.” His hospital, Alliance Healthcare Hospital, was one of the first to win the new Rural Emergency Hospital designation in early 2023. He laid off staff and shut down his inpatient beds. Then, CMS officials called to tell him they had made a mistake.
“And I said, ‘Wait a minute,’” Williams said. The hospital, which is about an hour south of Memphis, Tennessee, doesn’t meet the current criteria of rural, they told him. Williams, an internal medicine doctor, bought the hospital in 1999 and has been trying to keep it running since.

Federal regulators are now asking Williams to convert the facility into another type of Medicare payment model, such as the sole community hospital with inpatient beds that it was before. Williams said that would be difficult: “What kind of transition can I make, especially with reduced services?”
In Keokuk, the hospital fits the current requirements. Insight Health Group, the Michigan company that bought the shuttered facility last March, plans to apply for the new federal designation as soon as it obtains state permits under new Iowa regulations tailored to rural emergency hospitals. It would be the first such hospital in the state.
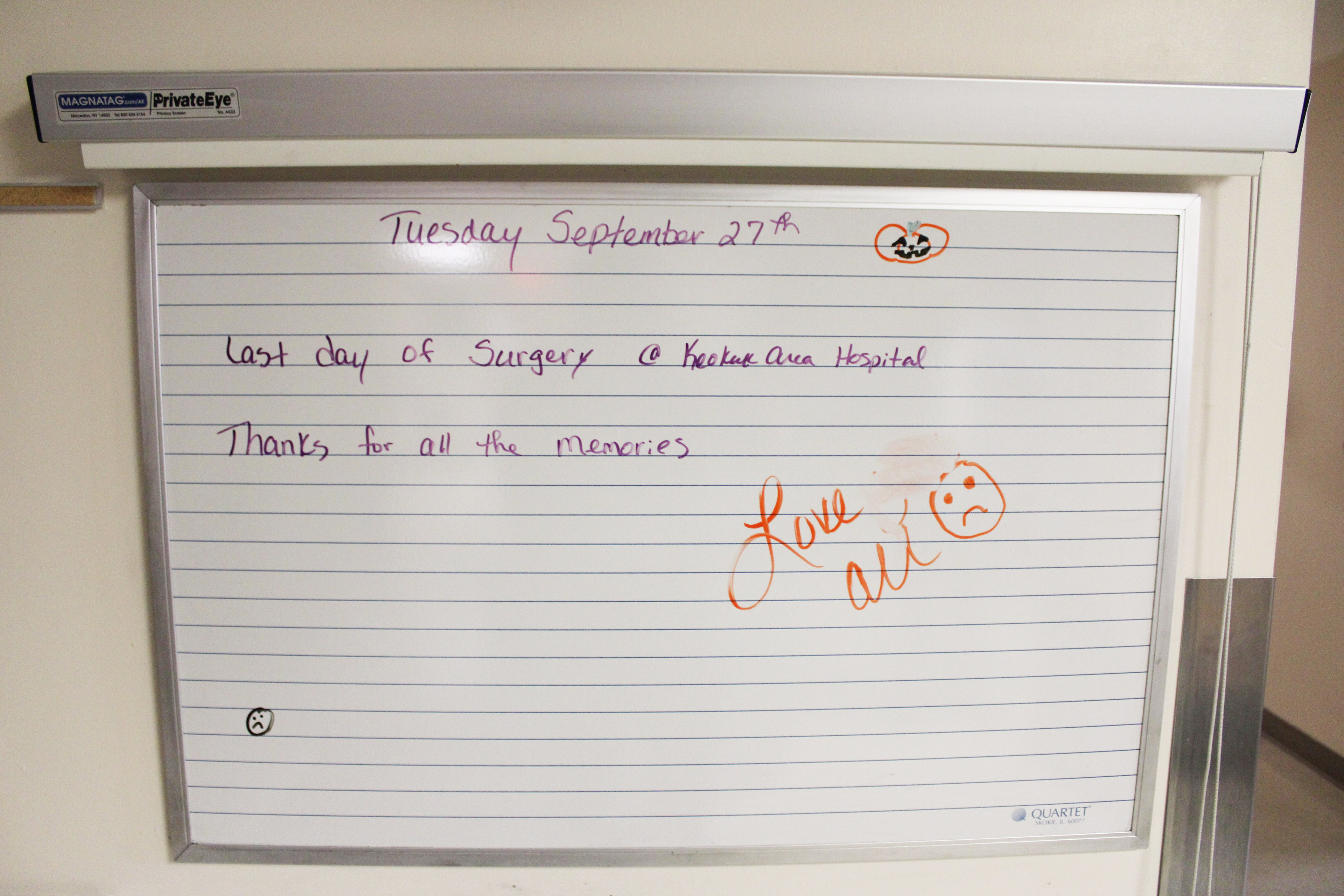
Like many other rural hospitals struggling to survive, Keokuk’s shuttered several key departments years ago, including its birthing and inpatient psychiatric units. In 2021, the last full year it was open, the hospital averaged fewer than three inpatients per night, according to data posted by the Iowa Hospital Association.
More than half of the three-story building would remain mothballed if the facility reopened under the new designation, but the emergency department could serve patients again as soon as late summer, said Atif Bawahab, Insight’s chief strategy officer.
Bruce Mackie has worked 32 years at the hospital, including 10 years as director of plant operations. The new owners kept him on to watch over the building. Beds, high-tech scanners, and lab equipment remain, but most of the clocks have stopped. “It’s spooky,” he said.
Even if the services are more limited than before, Mackie said, “everybody wants the hospital to reopen. This city needs an ER.”








