FORT SCOTT, Kan. — One Monday in February, 65-year-old Karen Endicott-Coyan gripped the wheel of her black 2014 Ford Taurus with both hands as she made the hour-long drive from her farm near Fort Scott to Chanute. With a rare form of multiple myeloma, she requires weekly chemotherapy injections to keep the cancer at bay.
She made the trip in pain, having skipped her morphine for the day to be able to drive safely. Since she sometimes “gets the pukes” after treatment, she had her neighbor and friend Shirley Palmer, 76, come along to drive her back.
Continuity of care is crucial for cancer patients in the midst of treatment, which often requires frequent repeated outpatient visits. So when Mercy Hospital Fort Scott, the rural hospital in Endicott-Coyan’s hometown, was slated to close its doors at the end of 2018, hospital officials had arranged for its cancer clinic — called the “Unit of Hope” — to remain open.
Then “I got the email on Jan. 15,” said Reta Baker, the hospital’s CEO. It informed her that Cancer Center of Kansas, the contractor that operated and staffed the unit, had decided to shut it down too, just two weeks later.
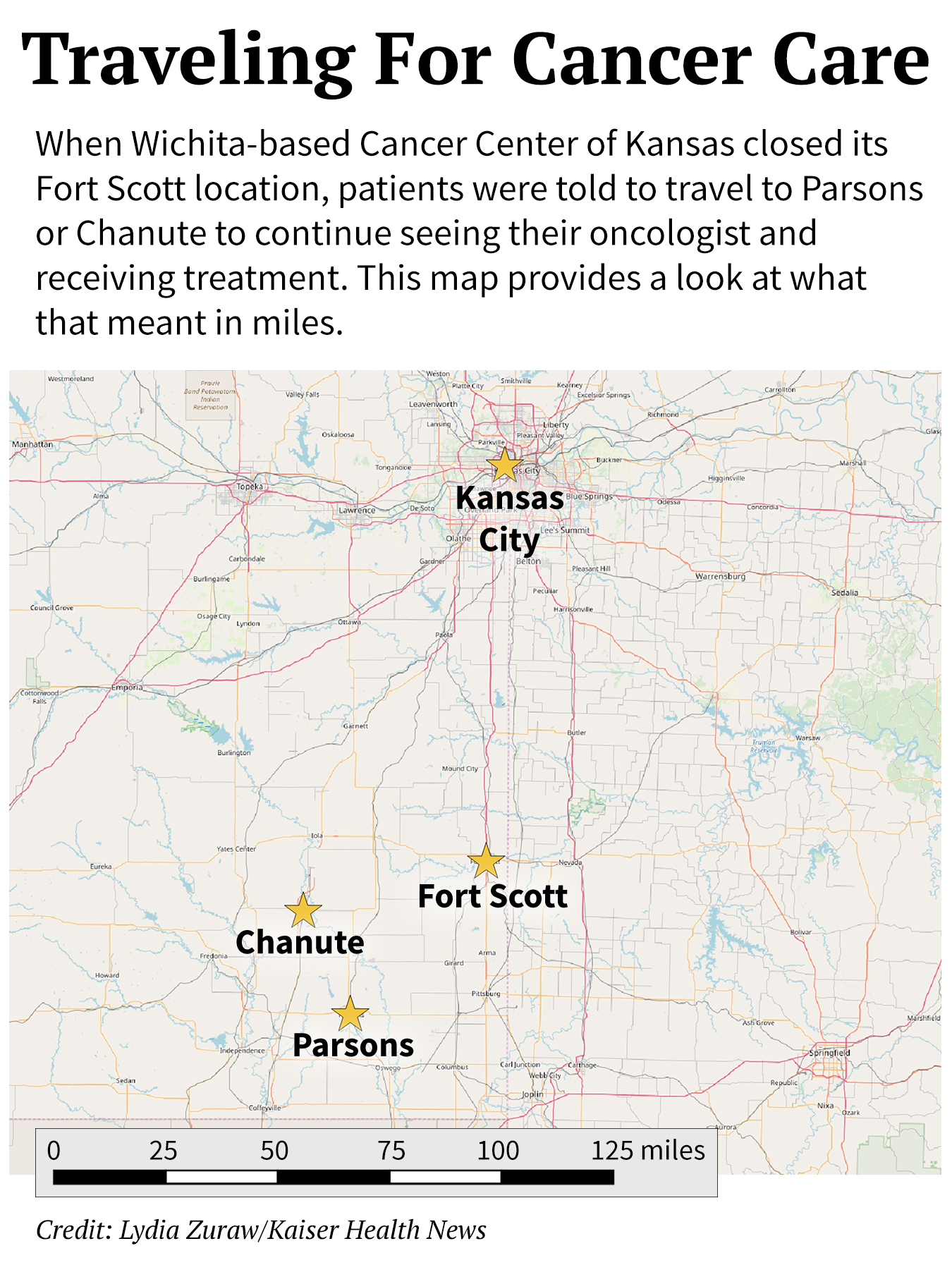
“There are too many changes in that town” to keep the cancer center open, Yoosaf “Abe” Abraham, chief operating officer of the Cancer Center of Kansas, later told KHN. He added that patients would be “OK” because they could get treated at the center’s offices in Chanute and Parsons.
From Fort Scott, those facilities are 50 and 63 miles away, respectively.
For Endicott-Coyan and dozens of other cancer patients, the distance meant new challenges getting lifesaving treatment. “You have a flat tire, and there is nothing out here,” Endicott-Coyan said, waving her arm toward the open sky and the pastures dotted with black Angus and white-faced Hereford cattle on either side of the shoulderless, narrow highway she now must drive to get to her chemo appointment.

When the cancer clinic at Mercy Hospital Fort Scott closed in January 2019, cancer patients such as Karen Endicott-Coyan had to continue their treatments in different locations. Endicott-Coyan has a rare form of multiple myeloma and now drives an hour from her farm near Fort Scott, Kan., to Chanute, Kan., for weekly chemotherapy injections.(Christopher Smith for KHN)
Nationwide, more than 100 rural hospitals have closed since 2010. In each case, a unique but familiar loss occurs. Residents, of course, lose health care services as wards are shut and doctors and nurses begin to move away.
But the ripple effect can be equally devastating. The economic vitality of a community takes a blow without the hospital’s high-paying jobs and it becomes more difficult for other industries to attract workers who want to live in a town with a hospital. Whatever remains is at risk of withering without the support of the stabilizing institution.
The 7,800 residents of Fort Scott are reeling from the loss of their 132-year-old community hospital that was closed at the end of December by Mercy, a St. Louis-based nonprofit health system. Founded on the frontier in the 19th century and rebuilt into a 69-bed modern facility in 2002, the hospital had outlived its use, with largely empty inpatient beds, the parent company said. For the next year, Kaiser Health News and NPR will track how its citizens fare after the closure in the hopes of answering pressing national questions: Do citizens in small communities like Fort Scott need a traditional hospital for their health needs? If not a hospital, what then?
Traveling The Distance For Cancer Care
Reta Baker, the hospital’s president who grew up on a farm south of Fort Scott, understood that the hospital’s closure was unavoidable. She scrambled to make sure basic health care needs would be met. Mercy agreed to keep the building open and lights on until 2021. And Baker recruited a federally qualified health center to take over four outpatient clinics, including one inside the hospital; former employees were bought out and continue to operate a rehabilitation center; and the nonprofit Ascension Via Christi Hospital in Pittsburg reopened the emergency department in February.
But cancer care in rural areas, which requires specialists and the purchase and storage of a range of oncology drugs, presents unique challenges.
Rural cancer patients typically spend 66% more time traveling each way to treatment than those who live in more urban areas, according to a recent national survey by ASCO, the American Society of Clinical Oncology. Dr. Monica Bertagnolli, a cattle rancher’s daughter who is now chair of ASCO’s board, called this a “tremendous burden.” Cancer care, she explained, is “not just one visit and you’re done.”
ASCO used federal data to find that while about 19% of Americans live in rural areas, only 7% of oncologists practice there.
People in rural America are more likely to die from cancer than those in the country’s metropolitan counties, according to a Centers for Disease Control and Prevention report in 2017. It found 180 cancer deaths per 100,000 people a year in rural counties, compared with 158 deaths per 100,000 in populous metropolitan counties.
The discrepancy is partly because habits like smoking are more common among rural residents, but the risk of dying goes beyond that, said Jane Henley, a CDC epidemiologist and lead author of the report. “We know geography can affect your risk factors, but we don’t expect it to affect mortality.”
From an office inside a former Mercy outpatient clinic, Fort Scott’s cancer support group, Care to Share, continues its efforts to meet some of the community’s needs — which in some ways have increased since the Unit of Hope closed. It provides Ensure nutritional supplements, gas vouchers and emotional support to cancer patients.
Lavetta Simmons, one of the support group’s founders, said she will have to raise more money to help people pay for gas so they can drive farther to treatments. Last year, in this impoverished corner of southeastern Kansas, Care to Share spent more than $17,000 providing gas money to area residents who had to travel to the Mercy hospital or farther away for care.

According to the U.S. Centers for Disease Control and Prevention, cancer kills more people in rural America than in the country’s metropolitan counties — 180 deaths per 100,000 people in rural counties, compared with 158 deaths per 100,000 in highly populated metropolitan counties.(Sarah Jane Tribble/KHN)
The group expects to spend more on gas this year, having spent nearly $6,000 during the first four months of 2019.
And the reserves of donated Ensure from Mercy are running out, so Simmons is reaching out to hospitals in nearby counties for help.
With Mercy Hospital Fort Scott closed, the likelihood of residents here dying from their cancer will grow, experts worry, because it’s that much harder to access specialists and treatments.
Krista Postai, who took over the Fort Scott hospital’s four primary care clinics, said it’s not unusual for her staff to “see someone walk in [with] end-stage cancer that they put off because they didn’t have money, they didn’t have insurance, or it’s just the way you are. … We wait too long here.”
‘If They Can’t Cure Me, I’m Done’
Art Terry, 71, a farmer and Vietnam veteran, was one of them. Doctors discovered Terry’s cancer after he broke a rib while baling hay. When they found a mass below his armpit, it was already late-stage breast cancer that had metastasized to his bones.
With his twice-weekly chemotherapy treatment available in the “Unit of Hope,” Terry spent hours there with his son and grandchildren telling stories and jokes as if they were in their own living room. The nurses began to feel like family, and Terry brought them fresh eggs from his farm.
“Dad couldn’t have better or more personalized care anywhere,” said his son, Dwight, bleary-eyed after a factory shift.
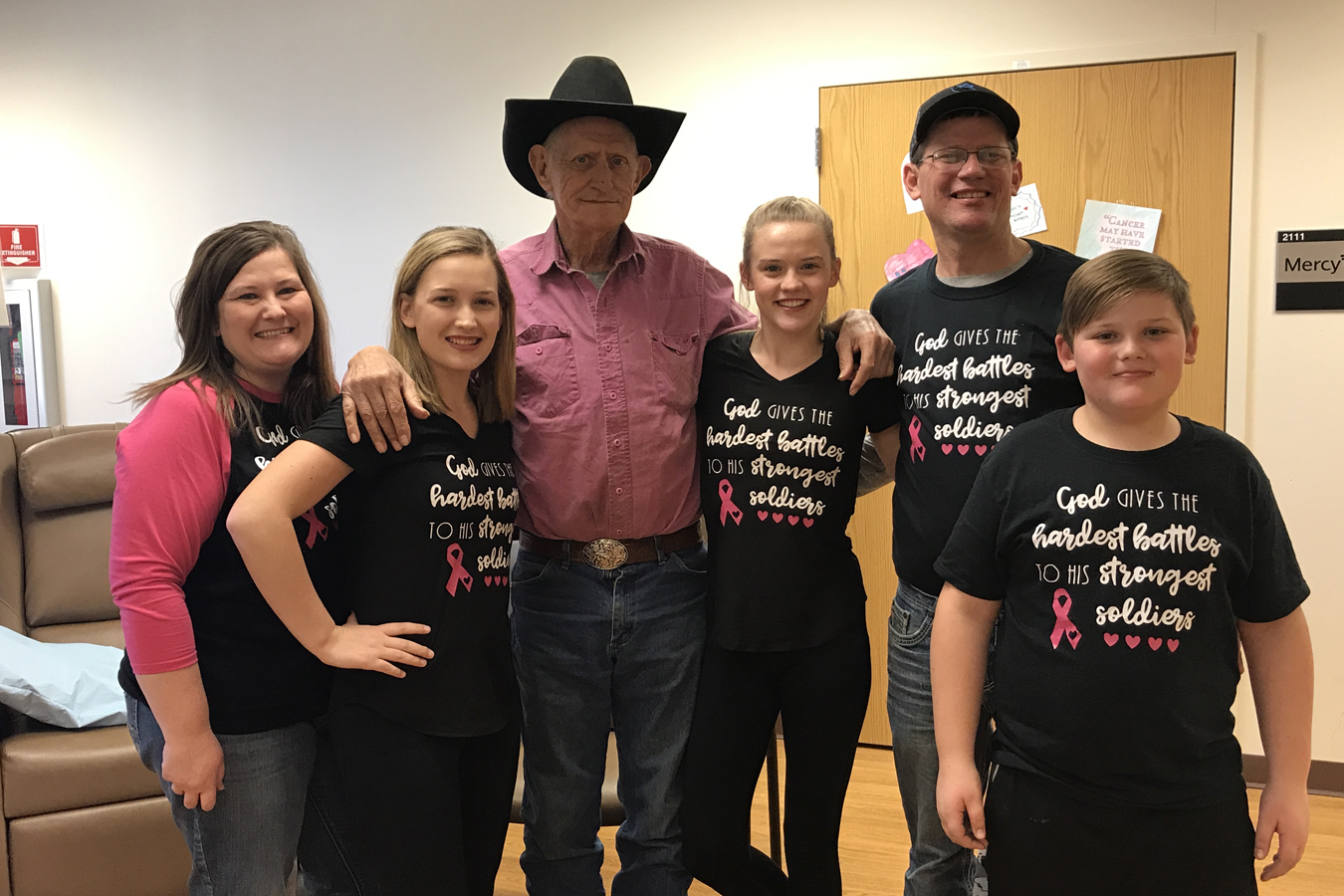
Art Terry, center, stands for a family photo at the Mercy Hospital Fort Scott cancer unit before its January closure. From left are Terry’s daughter-in-law, Sabrina; granddaughters Aubry and Shaylee; son Dwight; and grandson Blaiton.(Courtesy of Dwight Terry)
Terry knew it was difficult to find trustworthy cancer care. The shortage of cancer specialists in southeastern Kansas meant that many, including Mercy Hospital Fort Scott’s patients, counted on traveling oncologists to visit their communities once or twice a week.
Wichita-based Cancer Center of Kansas has nearly two dozen locations statewide. It began leasing space in Fort Scott’s hospital basement in the mid-2000s, the center’s Abraham said. The hospital provided the staff while the Cancer Center of Kansas paid rent and sent roving oncologists to drop in and treat patients.
At its closing, the Unit of Hope served nearly 200 patients, with about 40% of them on chemotherapy treatment.
When Art Terry was diagnosed, his son tried to talk to him about seeking treatment at the bigger hospitals and academic centers in Joplin, Mo., or the Kansas City area. The elder Terry wasn’t interested. “He’s like, ‘Nope,’” Dwight Terry recalled. “I’m going right there to Fort Scott. If they can’t cure me, I’m done. I’m not driving.’”
In the end, as the elder Terry struggled to stay alive, Dwight Terry said he would have driven his father the hour to Chanute for treatment. Gas — already a mounting expense as they traveled the 20 miles from the farm near tiny Prescott, Kan., to Fort Scott — would be even more costly. And the journey would be taxing for his father, who traveled so little over the course of his life that he had visited Kansas City only twice in the past 25 years.
As it turned out, the family never had to make a choice. Art Terry’s cancer advanced to his brain and killed him days before the hospital’s cancer unit closed.
What Happens Next?
As Endicott-Coyan and her friend Palmer drove to Chanute for treatment, they passed the time chatting about how the hospital’s closure is changing Fort Scott. “People started putting their houses up for sale,” Palmer said.
Like many in Fort Scott, they had both spent their days at the Fort Scott hospital. Endicott-Coyan worked in administration for more than 23 years; Palmer volunteered with the auxiliary for six years.

Debbie Endicott, Karen Endicott-Coyan’s sister-in-law, drives to chemotherapy in Chanute, Kan. The trip takes an hour on mostly narrow, two-lane highways from Endicott-Coyan’s home south of Fort Scott. “You can see there are no gas stations, there is nothing on the way,” Endicott-Coyan says. “There isn’t anything.”(Sarah Jane Tribble/KHN)
The hospital grew with the community. But as the town’s fortunes fell, it’s perhaps no surprise that the hospital couldn’t survive. But the intertwined history of Mercy and Fort Scott is also why its loss hit so many residents so hard.
Fort Scott began in 1842 when the U.S. government built a military fort to help with the nation’s westward expansion. Historians say Fort Scott was a boomtown in the years just after the Civil War, with its recorded population rising to more than 10,000 as the town competed with Kansas City to become the largest railroad center west of the Mississippi. The hospital was an integral part of the community after Sisters of Mercy nuns opened a 10-bed hospital in 1886 with a mission to serve the needy and poor. Baker, Mercy Hospital Fort Scott’s president, said the cancer center was an extension of that mission.
The Unit of Hope began operating out of the newest hospital building’s basement, which was “pretty cramped,” Baker said. As cancer treatments improved, it grew so rapidly that Mercy executives moved it to a spacious first-floor location that had previously been the business offices.
“Our whole purpose when we designed it was for it to be a place where somebody who was coming to have something unpleasant done could actually feel pampered and be in a nice environment,” Baker said.
The center, with its muted natural grays and browns, had windows overlooking the front parking lot and forested land beyond. Every patient could look out the windows or watch their personal television terminal, and each treatment chair had plenty of space for family members to pull up chairs.

Endicott-Coyan and her husband, John Coyan, laugh while sitting in their kitchen. John, 74, began showing signs of dementia in 2015. Together, they run a cow-calf operation on 240 acres south of Fort Scott and go to church every Sunday. (Christopher Smith for KHN)

Endicott-Coyan worked for nearly 24 years in the administration offices at Mercy Hospital Fort Scott, specializing in reimbursement issues. Diagnosed with cancer in October 2015, Endicott-Coyan receives weekly chemo treatment and says she experiences a lot of fatigue. “It’s 2019 and I’m still here and I’m still fighting,” she says. (Christopher Smith for KHN)
When Endicott-Coyan and Palmer arrived at the Cancer Center of Kansas clinic in Chanute in February, things looked starkly different. Patients entered a small room through a rusted back door. Three brown infusion chairs sat on either side of the entry door and two television monitors were mounted high on the walls. A nurse checked Endicott-Coyan’s blood pressure and ushered her back to a private room to get a shot in her stomach. She was ready to leave about 15 minutes later.
The center’s Abraham said the Chanute facility is “good for patients for the time being” and not a “Taj Mahal” like Mercy’s Fort Scott hospital building, which he said was too expensive to maintain. Cancer Center of Kansas plans to open a clinic at a hospital in Girard, which is about 30 miles from Fort Scott, he said.
Some oncology doctors would say driving is not necessary. Indeed, a few health care systems across the country, such as Sanford Health in South Dakota and Thomas Jefferson University Hospitals in Pennsylvania, are administering some chemotherapy in patients’ homes. Oncologist Adam Binder, who practices at Thomas Jefferson in Philadelphia, said “over 50% of chemotherapy would be safe to administer in the home setting if the right infrastructure existed.”
But the infrastructure — that is, the nurses who would travel to treat patients and a reimbursement model to pay for such care within our complex health care system — is not yet in place.
Back in the car, Palmer took the wheel and Endicott-Coyan began planning for future cancer treatments in the void left by Mercy Hospital Fort Scott’s closure. “I put a note on Facebook today and said, ‘OK, I have drivers for the rest of February; I need drivers for March!’”
This is the second installment in KHN’s year-long series, No Mercy, which follows how the closure of one beloved rural hospital disrupts a community’s health care, economy and equilibrium.







