Government spending on “compounded” drugs that are handmade by retail pharmacists has skyrocketed, drawing the attention of federal investigators who are raising fraud and overbilling concerns.
Spending on these medications in Medicare’s Part D program, for example, rose 56 percent last year, with some of the costliest products, including topical pain creams, priced at hundreds or thousands of dollars per tube. The federal workers’ compensation program has also seen a recent spike in spending.
The spending jump, along with a sharp increase in the number of patients getting the compounded drugs “may indicate an emerging fraud trend,” said Miriam Anderson, who helped oversee a June report on the Medicare spending by the inspector general’s office at the Department of Health and Human Services.
Some of the prescriptions may not have been medically necessary — or even dispensed at all, notes the report, which also details recent fraud cases brought by U.S. attorneys in several states.
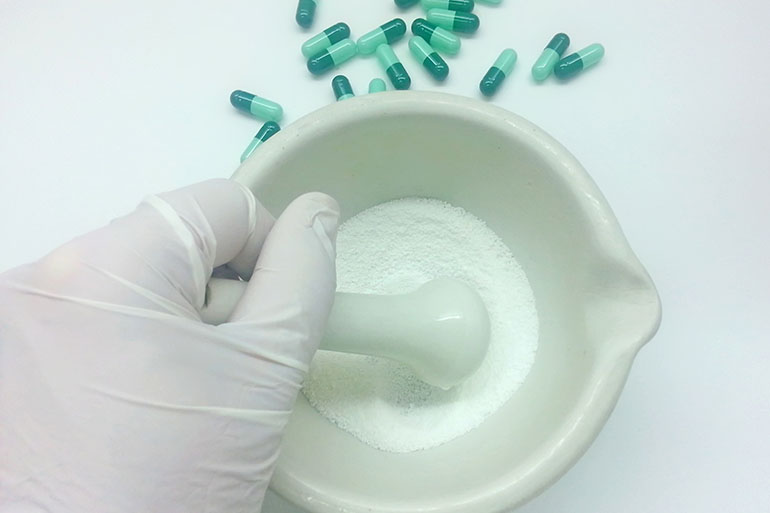
The practice of compounding drugs, which is done by mixing drugs in pharmacies or special compounding centers by licensed pharmacists, is as old as the pharmacy profession itself. By creating specifically tailored medications, compounding is aimed at patients who can’t take commercially available, FDA-approved medications.
But use among Medicare beneficiaries and federal employees in workers’ compensation insurance plans has recently soared, according to Anderson’s report and a separate Postal Service inspector general’s study of the workers’ comp program released last spring.
Similar run-ups in spending for compounded drugs were also noted by private-sector benefit managers in recent years.
In Medicare’s drug program, known as Part D, the number of Medicare beneficiaries getting compounded drugs has grown 281 percent since 2006 to nearly 280,000 in 2015. Spending on such drugs in Medicare’s Part D grew 625 percent between 2006 and 2015, to $509 million, according to the OIG report. That is still a tiny fraction of the program’s total spending on drugs.
The fastest-growing category of compounded drugs are topical creams and gels, often used for pain. Spending on those increased 3,466 percent in the Medicare program since 2006, the report said, while the average cost per prescription hit $331, up from $40 in 2006.
A large spike in spending for compounded drugs led the U.S. Postal Service to try to hold back payments for its share of federal workers’ compensation costs last year, saying the agency overseeing the program had failed to more strictly police the use of such drugs. It eventually paid.
Overall, the federal government’s worker’s compensation program, which includes the Postal Service, saw spending on compounded medications grow from $2.35 million in fiscal 2011 to $214 million in fiscal 2015, according to the Department of Labor, which oversees the program.
New rules from the DOL went into effect July 1, aimed at slowing the spending. Among other changes, the agency will now limit initial prescriptions to 90 days.
While legitimately prescribed compounded drugs “can dramatically improve a patients’ quality of life,” it is also important to have “proper controls around billing,” said John Voliva, executive vice president of the International Academy of Compounding Pharmacists, last week in a written statement. The HHS inspector general’s report demonstrated that such controls “are not in place,” he said.
Benefits Vs. Drawbacks
The studies come amid ongoing scrutiny of the drug compounding industry, particularly following a meningitis outbreak that killed 64 Americans in 2012. Those deaths were linked to a Massachusetts pharmacy that sold tainted injectable medications.
Following that outbreak, some states tightened their oversight of such pharmacies, particularly those producing products that must be sterile.
Compounding pharmacies are generally overseen by state boards of pharmacy, and the drugs they produce are not considered FDA approved. The agency does get involved, however, when it is concerned that pharmacies might not be making medications properly or have started to mass produce treatments, rather than preparing them for individual patients.
When prescribed appropriately, compounded drugs allow patients who can’t take or tolerate commercially prepared products to have special formulations mixed just for them. Patients who can’t swallow pills, for example, can get liquid formulations or those allergic to certain dyes can get products made without them.
And sometimes such drugs can be more cost-effective.
When Turing Pharmaceuticals raised the price of a drug used for patients with compromised immune systems from $13.50 a pill to $750 last year, for example, one of the nation’s largest pharmacy benefit managers partnered with a compounding pharmacy to produce its own version for $1 a pill, said Glen Stettin, senior vice president for clinical research of Express Scripts.
“Some compounding we should be happy for,” said Stettin.
But his organization nonetheless has sharply toughened its rules about what pharmacy-made products it will cover after seeing a sharp increase in spending that started in 2012.
Nationally, since 2012, pharmacies have been required to report all the ingredients they used to make a compounded drug. The idea was to provide insurers with more information about what they were being billed for and to make sure there were no hidden ingredients.
The effect that had on drug prices is up for debate. Stettin and others say a few unscrupulous pharmacies began adding more ingredients so they could charge more.
“They are [creating] combinations of things that have never been tested together,” said Stettin. “We saw a diaper cream that was billed at $1,000, where a patient could get one over the counter for $2.50.”
In California, federal investigators say a marketer for one pharmacy paid doctors to write prescriptions for compounded pain creams formulated to include a “five-pack” of the most expensive ingredients. Then the pharmacy could bill California’s worker’s compensation program $3,000 per tube for creams it cost about $20 to make, according to a federal indictment filed in June.
In Florida, federal prosecutors also in June unsealed an indictment against a doctor who allegedly was given kickbacks — including a $72,000 BMW — for sending prescriptions to a particular pharmacy, which then billed Tricare, Medicare and other government health programs for compounded creams. Prices ranged from about $900 to $21,000 for a one-month supply, according to court documents.
To combat rising spending, Express Scripts in 2014 drew up a list of about 1,000 ingredients used by compounders for which it would no longer pay, saying they were high priced and weren’t any safer or more effective than other treatments. Many of its clients, including the military health program Tricare, have incorporated that list into their health plans.
Since the limit, Express Scripts says it has seen its clients’ spending on pharmacy-made drugs fall sharply. The list has also prompted two antitrust lawsuits filed against Express Scripts in federal court by compounding pharmacies.
Awaiting Action
What actions Medicare will take — and the effectiveness of a July 1 change in how such medications are paid for in the federal compensation program — remain unclear. The Medicare report does not make any recommendations, although investigators expect to issue a follow up report that will.
In its March report, the inspector general criticized a lack of action by the Labor Department to address the growing spending, saying that it estimated the Postal Service “has incurred over $81.8 million in excessive compound drug costs and nearly $4.1 million in excessive administrative fees” for the past two fiscal years.
Following that, Labor issued new rules it says will “contain the cost of compound drugs … but still allow for appropriate medical treatment,” according to Leonard J. Howie III, director of the Office of Workers’ Compensation Programs.
KHN’s coverage of prescription drug development, costs and pricing is supported in part by the Laura and John Arnold Foundation.