A bill pending in California’s legislature to ratchet up oversight of private equity investments in health care is receiving enthusiastic backing from consumer advocates, labor unions, and the California Medical Association, but drawing heavy fire from hospitals concerned about losing a potential funding source.
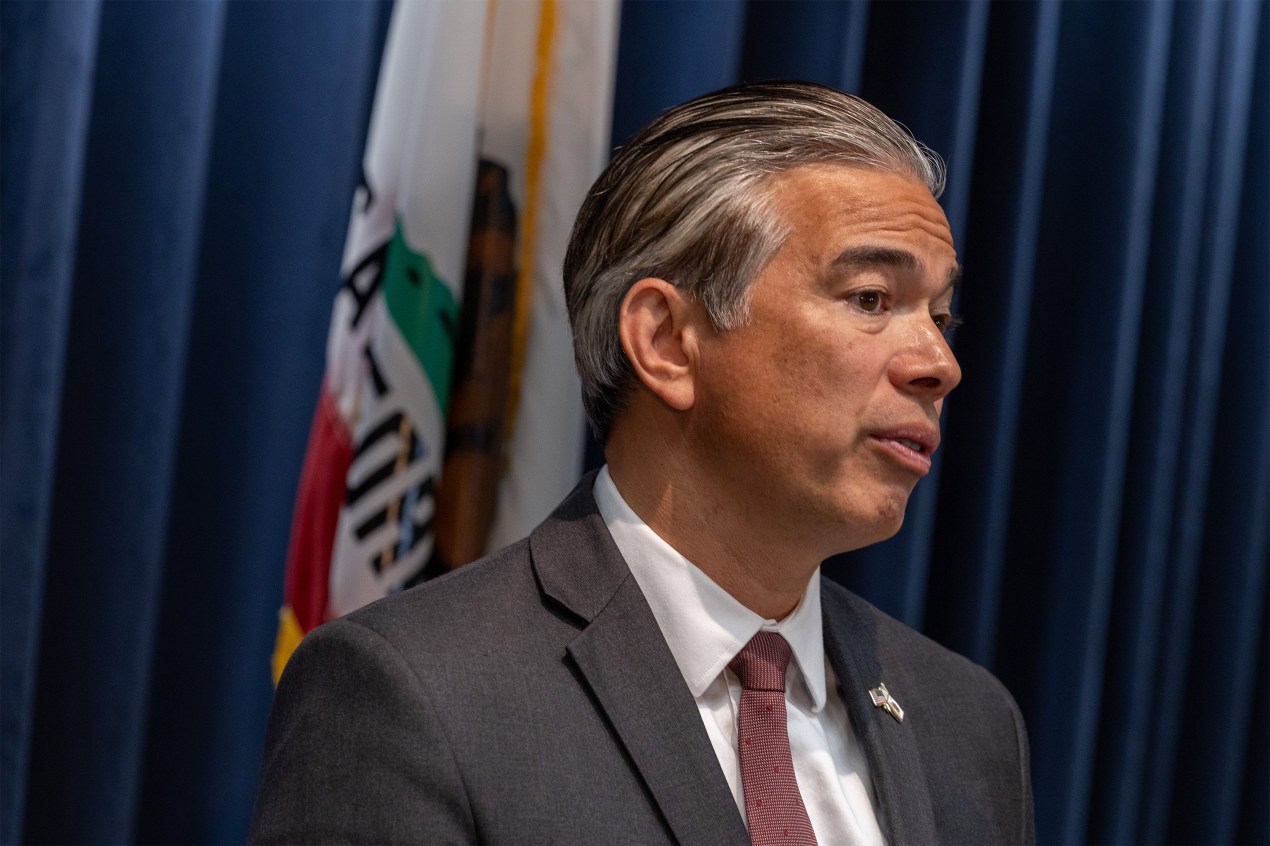
The legislation, sponsored by Attorney General Rob Bonta, would require private equity groups and hedge funds to notify his office of planned purchases of many types of health care businesses and obtain its consent. It also reinforces state laws that bar nonphysicians from directly employing doctors or directing their activities, which is a primary reason for the doctor association’s support.
Private equity firms raise money from institutional investors such as pension funds and typically acquire companies they believe can be run more profitably. Then they look to boost earnings and sell the assets for multiples of what they paid for them.
That can be good for future retirees and sometimes for mismanaged companies that need a capital infusion and a new direction. But critics say the profit-first approach isn’t good for health care. Private equity deals in the sector are coming under increased scrutiny around the country amid mounting evidence that they often lead to higher prices, lower-quality care, and reduced access to core health services.
Opponents of the bill, led by the state’s hospital association, the California Chamber of Commerce, and a national private equity advocacy group, say it would discourage much-needed investment. The hospital industry has already persuaded lawmakers to exempt sales of for-profit hospitals from the proposed law.
“We preferred not to make that amendment,” Bonta said in an interview. “But we still have a strong bill that provides very important protections.”
The legislation would still apply to a broad swath of medical businesses, including clinics, physician groups, nursing homes, testing labs, and outpatient facilities, among others. Nonprofit hospital deals are already subject to the attorney general’s review.
A final vote on the bill could come this month if a state Senate committee moves it forward.
Nationally, private equity investors have spent $1 trillion on health care acquisitions in the past decade, according to a report by The Commonwealth Fund. Physician practices have been especially attractive to them, with transactions growing sixfold in a decade and often leading to significant price increases. Other types of outpatient services, as well as clinics, have also been targets.
In California, the value of private equity health care deals grew more than twentyfold from 2005 to 2021, from less than $1 billion to $20 billion, according to the California Health Care Foundation. Private equity firms are tracking the pending legislation closely but so far haven’t slowed investment in California, according to a new report from the research firm PitchBook.
Multiple studies, as well as a series of reports by KFF Health News, have documented some of the difficulties created by private equity in health care.
Research published last December in the Journal of the American Medical Association showed a larger likelihood of adverse events such as patient infections and falls at private equity hospitals compared with others. Analysts say more research is needed on how patient care is being affected but that the impact on cost is clear.
“We can be almost certain that after a private equity acquisition, we’re going to be paying more for the same thing or for something that’s gotten worse,” said Kristof Stremikis, director of Market Analysis and Insight at the California Health Care Foundation.
Most private equity deals in health care are below the $119.5 million threshold that triggers a requirement to notify federal regulators, so they often slide under the government radar. The Federal Trade Commission is stepping up scrutiny, and last year it sued a private equity-backed anesthesia group for anticompetitive practices in Texas.
Lawmakers in several other states, including Connecticut, Minnesota, and Massachusetts, have proposed legislation that would subject private equity deals to greater transparency.
Not all private equity firms are bad operators, said Assembly member Jim Wood, a Democrat from Healdsburg, but review is essential: “If you are a good entity, you shouldn’t fear this.”
The bill would require the attorney general to examine proposed transactions to determine their impact on the quality and accessibility of care, as well as on regional competition and prices.
Critics note that private equity deals are often financed with debt that is then owed by the acquired company. In many cases, private equity groups sell off real estate to generate immediate returns for investors and the new owners of the property then charge the acquired company rent.
That was a factor in the financial collapse of Steward Health Care, a multistate hospital system that was owned by the private equity firm Cerberus Capital Management from 2010 to 2020, according to a report by the Private Equity Stakeholder Project, a nonprofit that supports the California bill. Steward filed for Chapter 11 bankruptcy in May. “Almost all of the most distressed US healthcare companies are owned by private equity firms,” according to another study by the group.
Opponents of the legislation argue it would dampen much-needed investment in an industry with soaring operating costs. “Our concern is that it will cut off funding that can improve health care,” said Ned Wigglesworth, a spokesperson for Californians to Protect Community Health Care, a coalition of groups fighting the legislation. The prospect of having to submit to a lengthy review by the attorney general, he said, would create “a chilling effect on private funders.”
Proponents of private equity investment point to what they say are notable successes in California health care.
Children’s Choice Dental Care, for example, said in a letter to state senators that it logs over 227,000 dental visits annually, mostly with children on Medi-Cal, the health insurance program for low-income Californians. “We have been able to expand to 25 locations, because we have been able to access capital from a private equity firm,” the group wrote.
Ivy Fertility, with clinics in California and eight other states, said in a letter to state senators that private investment has expanded its ability to provide fertility treatments at a time when demand for them is increasing.
Researchers note that private equity investors are hardly alone when it comes to health care profiteering, which extends even to nonprofits. Sutter Health, a major nonprofit hospital chain, for example, settled for $575 million in a lawsuit brought by then-Attorney General Xavier Becerra, for unfair contracting and pricing.
“It’s helpful to look at ownership classes like private equity, but at the end of the day we should look at behavior, and anyone can do the things that private equity firms do,” said Christopher Cai, a physician and health policy researcher at Harvard Medical School. He added, though, that private equity investors are “more likely to engage in financially risky or purely profit-driven behavior.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.