Sumana Reddy, a primary care physician, struggles on thin financial margins to run Acacia Family Medical Group, the small independent practice she founded 27 years ago in Salinas, a predominantly Latino city in an agricultural valley often called “the salad bowl of the world.”
Reddy can’t match the salaries offered by larger health systems — a difficulty compounded by a widespread shortage of primary care doctors.
The shortage is tied largely to the lower pay and relative lack of prestige associated with primary care, making recruitment difficult. “It certainly is challenging to expose medical students early in their careers to the joys of this kind of integrated health care,” Reddy said. “The relationships we build and the care we provide truly allow people to live longer with a better quality of life.”
Hoping to increase revenue so Acacia can afford to pay more, Reddy has signed the practice up for alternative payment methods with health plans that offer bonuses for meeting certain primary care goals tied to child vaccinations, blood pressure control, and screenings for breast cancer, colorectal cancer, and mental health. Such pay-for-performance arrangements are among the many efforts by industry players and state officials to confront the problems plaguing primary care.
Medical students frequently opt not to go into primary care, and that’s not good for patients. People with regular primary care providers are more likely to get preventive care that avoids serious illnesses and feel more empowered to advocate for themselves. They’re also less likely to encounter language barriers, resort to costly emergency room visits, or forgo care.
Six years after the influential California Future Health Workforce Commission made a series of recommendations to plug a projected shortage of 4,100 primary care providers in 2030, a number of public and private initiatives have proliferated around the state to address the problem. They include new residency slots, debt forgiveness, waived medical school tuition, new ways of paying doctors, expanded nurse practitioner roles, and a statewide target to increase primary care spending. Hundreds of millions of taxpayer dollars have been allocated for some of these efforts.
But numerous academic experts and medical professionals believe those moves, while well intended, have been scattershot and insufficient. “The pieces are there,” said Monica Soni, chief medical officer of Covered California, the state’s Affordable Care Act health insurance marketplace. “I am worried we started a little too late, and I think it’s a little too siloed.”
A study published in 2022 by the California Health Care Foundation found that substantial progress had been made on some of those goals, including recruitment of students from low-income households and communities of color. A separate analysis from the foundation showed that, from 2020 to 2023, California jumped about 10 spots in a ranking of states by primary care residents and fellows per capita.
However, the latest state data shows nearly 15 million Californians live in areas without enough primary care providers to meet patient needs.
State budget constraints and potential federal spending cuts, especially to Medicaid, could exacerbate shortages in areas already desperate for clinicians and dampen hopes of building a robust primary care system that state officials and virtually everyone in the industry agree would be a strong defense against serious — and costly — illnesses. Federal cuts could also hit medical training and hospital systems.
“Many of us are very scared about threats from both the Trump administration and Republicans in Congress,” said Kevin Grumbach, a family community medicine professor at the University of California-San Francisco.
Acute Primary Care Shortages
California’s lack of primary care providers, including doctors, nurse practitioners, and physician assistants, is most acute in rural parts of the state, particularly in the north and the Central Valley. Entire rural counties, including Del Norte, Madera, Tulare, and Yuba, are designated shortage areas, according to state data. Some densely populated urban areas, including parts of Los Angeles, also confront shortages.
Many Californians face months-long waits for appointments or have to travel long distances or go to emergency rooms for nonurgent medical needs, which means hours spent in crowded waiting rooms for unnecessarily expensive care.
In Chico, 90 miles north of Sacramento, the emergency room at the only hospital in town has seen a sharp increase in patients over the past decade, due in part to a lack of primary care providers in the area.
“People who don’t have a primary care provider — which is a lot, because there are not enough — end up in the ER when they need routine care,” said David Alonso, a local internal medicine doctor. “The ER then says, ‘OK, you should follow up with your primary care provider,’ and they’re like, ‘We don’t have one.’”
Yalda Jabbarpour, director of the Robert Graham Center for Policy Studies, a health policy think tank, said failure to invest robustly in primary care has robbed the public of its benefits.
The field has historically been underfunded, accounting for less than 5% of national health care spending in 2022, according to the Milbank Memorial Fund, a national nonprofit focused on population health and health equity.
The consequences are clear.
The U.S. spends significantly more per capita on health care than other industrialized nations, and yet Americans aren’t any healthier. Chronic conditions such as heart disease, diabetes, arthritis, and Alzheimer's, as well as mental illness, account for 90% of the $4.5 trillion spent on health care every year.
Medical students, often faced with staggering educational debt, are increasingly choosing higher-paid specialties over primary care. The average salary of a family medicine physician is slightly over $300,000, compared with more than $565,000 for a cardiologist and over $763,000 for a neurosurgeon, according to one study.
“If you are going to pay over $300,000 to go to medical school, you want to be a neurosurgeon; you don’t want to be a family practice doctor,” said William Barcellona, executive vice president of government affairs at America’s Physician Groups, a Los Angeles-based professional association representing 360 medical groups and independent practice associations nationwide.
Barcellona said the Golden State’s high housing costs also make recruiting difficult.
But it’s not only pay that tempers enthusiasm for primary care. It’s also burnout from so many unpaid hours spent recording details of medical visits in electronic health records; haggling with insurance companies for treatment authorization; answering phone calls and emails from patients; or searching far and wide — often in a health care desert — for specialists with the right expertise.


Debby Lee, the daughter of Hmong immigrants from Laos, experienced this kind of frustration firsthand.
Cultural and linguistic barriers faced by her family motivated her to pursue internal medicine. Lee worked part of her residency at a community clinic serving Hmong in the Sacramento area. She loved the patients, as well as her co-workers. But she was burdened by outdated technology that limited the number of patients she could see. “I just saw myself kind of burning out being in that setting,” Lee said.
When the clinic invited her to stay, she declined, taking a job with a bigger health system.
Solutions to the Shortage
Besides residencies, other efforts support primary care.
The Health Plan of San Mateo offers grants to help medical practices retain and add to primary care staff. In exchange, the practices — some single physicians serving patients in California’s Medicaid program, Medi-Cal — must show they have increased their patient load and retained newly hired providers for five years.
The idea is to provide capital so doctors can hire the staff they need to run their practices efficiently, increase salaries, offer bonuses, and even take sabbaticals. Such efforts are consistent with one of the main thrusts of the 2019 workforce report: to increase investment in primary care.
California recently joined several other states, including Connecticut, Oklahoma, and Rhode Island, in setting a target to increase primary care spending. So far, those policies have yielded mixed results.
Late last year, California’s Office of Health Care Affordability set a target to make primary care account for 15% of total health care spending by 2034, more than double the current proportion. It imposes no requirements, relying on the goodwill of health plans to work with medical providers.
Greater spending on primary care would mean better pay and more people working in the field, said Richard Kronick, a public health professor at UC-San Diego and a member of the OHCA board. “That’s a big change. Will it happen? I don’t think anyone can predict the future with any certainty.”
Stephen Shortell, a professor emeritus of health policy and management at UC-Berkeley, said “some of that increase might occur, but at some point, it might need to be made mandatory.”
In its report, the workforce commission also cited the importance of alternative forms of primary care payment that offer extra cash for quality care. The affordability office has set targets to encourage such payment methods. The aim is to transform the system from one in which every medical service has a price tag to one that treats people holistically, and in which adherence to medical standards brings more money to doctors and their office staff.
Such arrangements are common among HMOs, though less so in primary care practices. Where they do exist, different health plans and other payers generally design them differently, which means primary care practices manage multiple payment models, adding to their administrative burden.

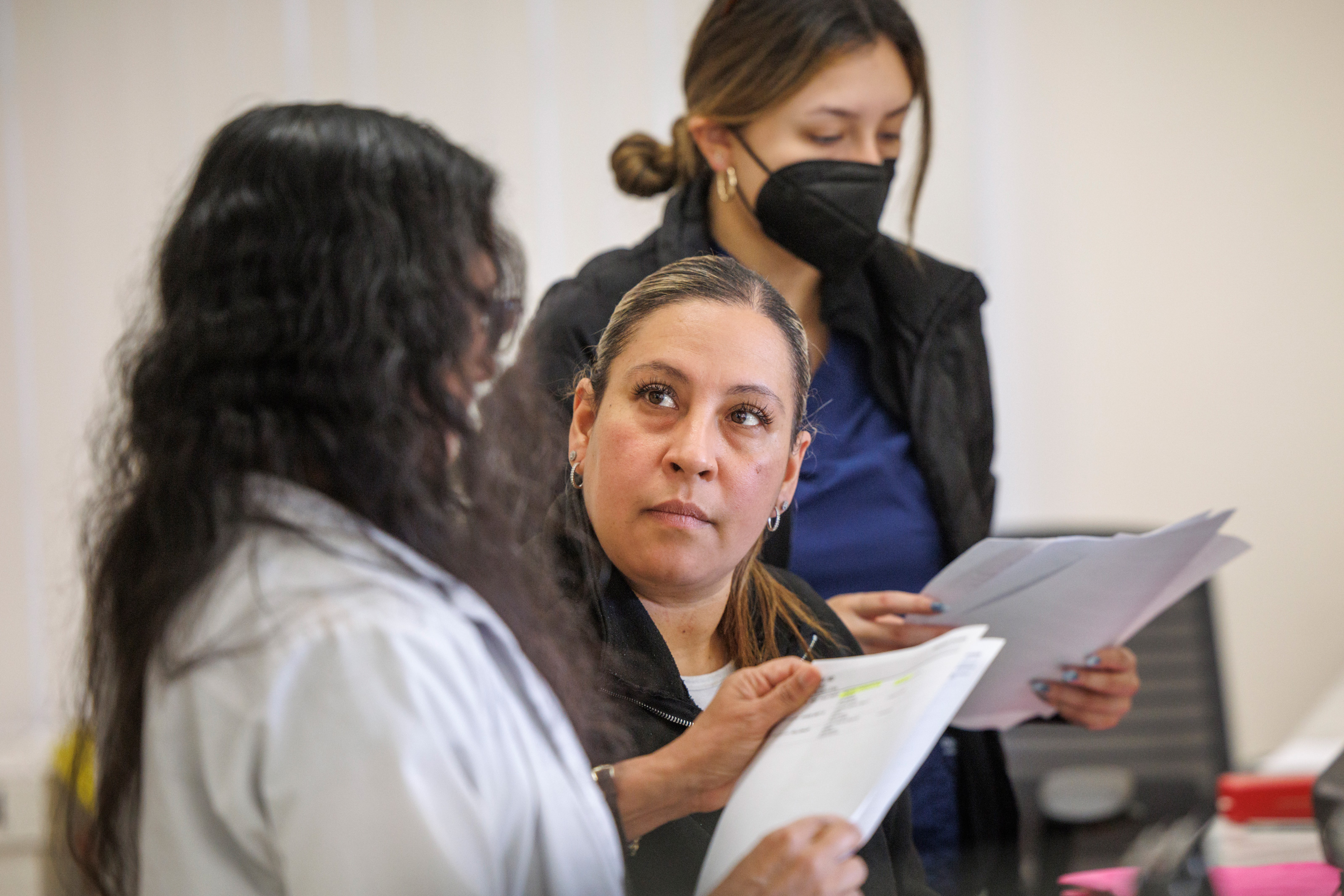
Reddy’s family practice is participating in a one-year demonstration project launched in January intended to reduce that burden by having multiple insurers work together in one payment plan.
The project brings together three large insurers — Health Net, Aetna, and Blue Shield of California — and 10 independent practices across the state with the goal of improving care while boosting revenue for the medical groups. It is administered by two industry groups, the Integrated Healthcare Association and the California Quality Collaborative.
On top of customary payments, either for services rendered or monthly per-member allotments, the medical practices receive bonuses for meeting targets or improving their performance on core measures.
Participating practices also receive monthly per-patient payments for “population health management,” which means managing the collective health of their patients. And they can search a single platform to find all their patients covered by one of the three plans.
In addition to extra payments and fewer administrative hassles, the health plans pay for a “practice coach,” whose job is to help primary care groups meet their targets and provide more seamless care.
The idea is to add more insurers and medical groups over time, said Todd May, Health Net’s medical director for commercial health plans, who is among those driving the project. “In addition to better outcomes, we’d like to see a stronger, more robust, and more satisfied primary care workforce,” he said.
Reddy hopes she can increase Acacia’s revenue by 20%, using the extra money from this and other pay-for-performance arrangements. That, she said, would enable her to raise pay for her staff and hire clinicians.
For many years, her practice has limited the number of patients it has accepted. But after searching for the better part of five years, Reddy has hired a doctor on a half-time basis and another is coming on board in June.
“This is the most hopeful I have felt in decades,” Reddy said.
Phillip Reese contributed to this report.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.








