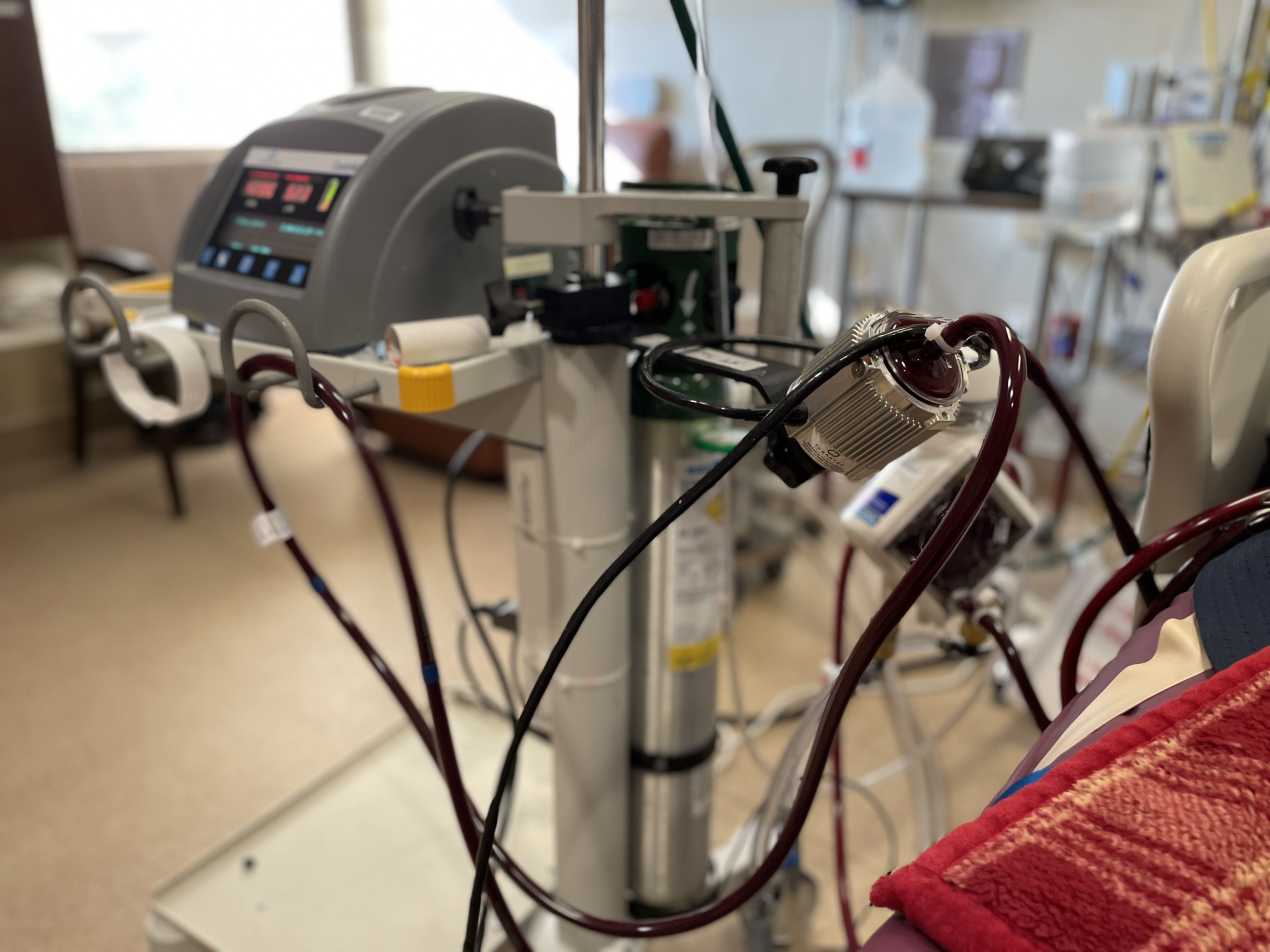
Speaking from his hospital bed at Vanderbilt University Medical Center in Nashville, Tennessee, James Perkinson’s voice was raspy. In February, he’d just been taken off ECMO, the last-ditch life support treatment in which a machine outside the body does the work of the heart and lungs.
Full recovery is expected to take a year or more for Perkinson.
“If it wasn’t for the ECMO and the doctors that were put in place at the right time with the right knowledge, I would not be here,” he said, with his wife, Kacie, by his side.
“Could there have been a miracle and he could have lived if he hadn’t gotten [ECMO]? Maybe. But the chances were absolutely slim to none,” Kacie said.
A new study from Vanderbilt shows she’s probably right about those chances.
During the surge of the delta variant of covid-19 late last summer, ECMO therapy was in short supply across the South. Vanderbilt’s unit was taking 10 to 15 calls a day from hospitals without ECMO looking for an open bed. Even patients’ families were calling on behalf of dying loved ones.
“‘There’s no beds. There’s no nurses. There’s no machines. There’s just not enough. We just physically can’t,’” nurse practitioner Whitney Gannon said she would tell people calling from hospitals around the South. “It’s the worst feeling in the world.”
But Gannon grew curious about what happened to the patients she had to turn down — especially those who were young and healthy, like Perkinson, who was 28. She started checking back, informally.
Many of them had died, including a pregnant woman.
So, within a matter of weeks, she helped launch an official study. And Gannon’s team started taking every call, even when no beds were available.
“We wanted to know: Is this patient truly medically eligible for ECMO? Would we provide ECMO? And if we didn’t, we wanted to know what happened to that patient,” Gannon said.
The results, published in the American Journal of Respiratory and Critical Care Medicine, are grim. Nearly 90% who couldn’t find a spot at an ECMO center died. And these patients were under 60 and previously healthy, with a median age of 40.
Over the course of the pandemic, hospitals have had difficulty deciding who gets priority when ECMO, which stands for extracorporeal membrane oxygenation, is in short supply. It’s not an exact science. And there are precious few ECMO beds, especially when some patients linger for months on the machine, only to die.
Perkinson was a good candidate since he’s young and — before falling ill with covid — relatively healthy. A machinist from Greenbrier, Tennessee, and a father of two, he caught covid after making an appointment to get his first dose of vaccine, he said.
Without vaccine protection, he didn’t fare well against the virus. He was put on a ventilator just after Christmas and within days stepped up to an available ECMO bed as his blood oxygen levels dropped.
For nearly two months, his blood flowed through a tube in his neck to the ECMO unit, which infused it with oxygen, took out the carbon dioxide, and sent it back into his body. He was sedated the entire time, increasing his risk of long-term organ damage and disability.
The use of ECMO spiked during the pandemic. Never has it been used so widely, but the data remains limited. And a study published in The Lancet in September 2021 found that the number of covid patients dying while on ECMO had increased 15% since the beginning of the pandemic.
Even early on, only half were surviving. And as the pandemic dragged on, more hospitals with less experience were using ECMO, and some expanded criteria to include older patients or those with risk factors like obesity who do not do as well.
Hospital capacity crunches have been central to the debate because ECMO requires a small village of nurses and respiratory therapists. And sometimes the patients stay on the therapy for months, not just weeks.
One patient currently at Vanderbilt, which has just seven ECMO beds, has been there since last year’s delta surge, said Dr. Jonathan Casey.
“So you can imagine how it doesn’t take much to fill this resource even during a small wave,” Casey said.
Even during the omicron surge, Casey said, Vanderbilt has turned down some transfer requests for ECMO.
While the odds of survival with critical covid patients are still roughly 50-50, the Vanderbilt study shows what happens if the therapy is unavailable.
“I’m trying to convince people that this is a resource worth investing in and then hoping people invest in those resources over time,” said Casey, the study’s senior author.
Until there is broader access to ECMO, Casey said, the country also needs to find a better way to decide who is prioritized for treatment, similar to how organ transplant allocation works. There is a national ECMO organization called the Extracorporeal Life Support Organization, but it doesn’t get involved with triaging patients yet.
Some hospitals will agree to try ECMO on someone over 70, if the family pushes hard enough. Others turn down patients over 50, especially if they have underlying diabetes or heart disease.
Small-scale cooperative efforts are underway. In Minnesota, hospitals have agreed to use the same strict patient criteria and a statewide referral process.
The decisions are still “ethically nuanced,” said Dr. Matthew Prekker, who helped set up the consortium before the pandemic emerged. Cooperation could mean giving an ECMO bed to a patient from across the state instead of someone in your own hospital.
The goal is simply for more patients to survive.
“It takes a lot of cooperation among health systems and state leadership,” he said. “But I think doctors and communities have more appetite for that now than they did before.”
This story is part of a partnership that includes WPLN, NPR, and KHN.