When the Institute of Medicine came out last month with a report saying almost every American will experience a medical diagnostic error, Leslie Michelson wasn’t surprised.
He runs Private Health Management, a Los Angeles based company that – for a substantial fee – helps patients figure out what’s wrong with them, often after an array of doctors have failed to do so. The firm gathers the client’s medical records, selects experts in the condition for which the patient has been diagnosed, refers biopsy results for second opinions – and often sends patients to meet with top-tier specialists. Sometimes, they find the patient doesn’t have the condition originally diagnosed. Other times, the diagnosis is correct, but the treatment is not. His firm’s services are costly, running into the tens of thousands of dollars.
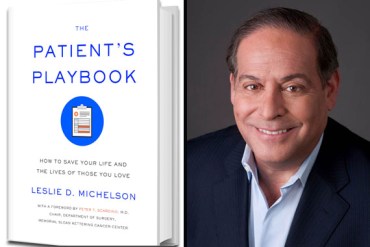
Leslie Michelson and his book, The Patient’s Playbook (Photo courtesy of Michelson)
But consumers can do this themselves, said Michelson, if they stop being passive about their medical care. He’s penned a book, The Patient’s Playbook: How to Save Your Life and the Lives of Those You Love. It offers a range of ideas on how to research doctors and conditions, while also outlining how important it is to have trusted family and friends as backups when serious illness strikes. Still, not each person who thinks he or she has an exotic disease actually does – and some of Michelson’s recommendations to reach out to top-tier superstar medical experts may prove daunting or unrealistic for the average consumer. KHN spoke with him about how to navigate the health system and avoid diagnostic errors. This interview has been edited for length.
What is diagnostic error and how common is it?
We don’t know precisely how common diagnostic error is because the essence of the problem is that it is difficult to measure [but] … we see it with incredible frequency. What is a diagnostic error? Someone being treated for the wrong cancer, for a disease they don’t have, … [for] back pain when [it’s not clear] whether the cause of the pain is a structural issue, a neurologic issue, an auto-immune condition or something else. And yet they’re going in with an intervention. It’s particularly painful with respect to cancers. When people are treated for the wrong cancer, they’re generally getting treatment that is totally ineffective. They get none of the benefit of the intervention, but all the side effects.
What are the three most important things a person can do to try to avoid a diagnostic error?
If you get a diagnosis, a significant diagnosis, it’s always important to see a physician with the exact expertise in what you have, particularly if it’s a rare condition.
Second is to get a second opinion. The carpenters have taught us this. Measure twice, cut once. And that’s for a piece of wood. You’re talking about determining an expensive, potentially complicated treatment program. If diagnosis is not measured twice – independently confirmed by a second pathologist – why engage in this entire potentially multi-year, multi-modality intervention unless you know exactly?
The third piece is to become an educated consumer. For all sorts of reasons, all of us are acculturated to be passive when it comes to our health, particularly when we’re sick. Figure out how to summon the courage and develop the confidence to partner with your physician. There are terrific resources online that everyone can use to understand whether their diagnosis is accurate.
Can you name some?
One of the best ones is the National Comprehensive Cancer Network. It’s a group of 26 major cancer centers that for the past two decades have developed treatment protocols for all the major cancers. You can find out the symptoms, the treatments and what indices will result in a diagnosis that’s accurate. Another great resource is something called Expertscape. They’ve taken all the medical articles over the past decades, organized them by disease and identified the authors of those articles. All you need to do is put in the name of that diagnosis, put in your zip code, put in a radius of how many miles you are prepared to travel, push search and it will identify for you the physicians who have done the most prominent research on that condition. Anyone can do it.
If many more people heeded your advice to seek second opinions and physicians with special expertise, wouldn’t those specialists be flooded with patients?
I think the dynamic would work fine if everyone were to become more effective consumers. In every other realm of our economy, when people become more effective consumers, the providers of services and goods become responsive. I think it would be a great thing if the most proficient surgeons, the most proficient diagnosticians, the very best dentists got the cases where they could really demonstrate their talent.
Reading your book can make one paranoid. What if my doctor is wrong? At what level should seek a second opinion?
Americans are fabulous consumers. We’re good at harnessing information. If it’s a significant issue that is being diagnosed, get a second opinion from an expert in exactly that condition. Even if it’s not, if that little nagging gut instinct says to you “this isn’t right,” act on it.
Are there other groups that help someone who doesn’t have tens of thousands to spend on private services like your firm’s?
Yes, there are so many resources [from] disease-specific foundations. You can get tremendous pamphlets, resources and recommendations for physicians. All of them are out there awaiting an email from you, a phone call from you.
I’m going to play devil’s advocate now. Isn’t there a risk, if patients follow your recommendations, that it would lead to additional tests and procedures that may not make a difference in their treatment or outcome, but would add costs to the patients and society?
No. Part of the reason we have overtesting or overtreatment problems in the U.S. is because of the structure of the reimbursement system. Physicians generally get paid more to do more. The second cause is patients that are too passive. When patients learn how to use the resources online to learn about their diseases and the fundamental importance of getting to experts in their precise condition, my experience is they will have the shortest line between the presentation of symptoms, the development of definitive diagnoses and the implementation of effective treatment plans. A lot of unnecessary costs – and the best estimates are that 30 percent of all health care spending is either unnecessary or counterproductive – are because patients aren’t going to specialists they need to.






