>> Can’t see the audio player above? Click here to download it.
Born just a year apart, Oliver Massengale and his brother Charles grew up together. Now, in a two-story home in Compton, California, they are growing old together. But Charles Massengale, 71, can do little on his own.
The former tree trimmer has severe brain damage from a 30-foot fall, as well as dementia, diabetes and high blood pressure. Six years ago, Oliver took over as his brother’s full-time caregiver, paid about $10 an hour by the state.
It was not a job he was trained to do.
“I didn’t have a clue,” said Oliver, a retired grounds manager at a college. “I was just so afraid of what I was doing.”
He constantly worried – about giving Charles the wrong medication, about him getting bedsores, about his blood pressure. And he had no idea how easily his brother could fall over. One day, he was cooking and Charles was on a stool at the kitchen counter.
“I heard BAM,” he said. “I turned around and he was on the kitchen floor.”
No overall training is required for the more than 400,000 caregivers in California’s $7.3 billion In-Home Supportive Services Program (IHSS) for low-income elderly and disabled residents. Without instruction even in CPR or first aid, these caregivers can quickly become overwhelmed and their sick or disabled clients can get hurt, according to interviews with caregivers, advocates and elder abuse experts.
The lack of training is “of enormous concern,” said Gary Passmore, a vice president of the Congress of California Seniors, an advocacy organization. “We are dealing with a lot of frail, elderly people.”
The need for in-home caregivers is rising as the elderly and disabled population grows. The demand for personal aides – most of whom work in the home — is expected to increase by 37% over the next decade, requiring about 1.3 million new positions, according to research published last year by the New-York based Paraprofessional Healthcare Institute, an advocacy group that also provides training.

Oliver Massengale took over as his brother’s full-time caregiver six years ago. He says he hasn’t had time for himself in years (Photo by Heidi de Marco/KHN).
The federal government is trying to meet that need by stepping up efforts to expand and train the work force. But for now, there are no federal training requirements for in-home-caregivers. It’s up to states to set them in Medicaid-funded programs like California’s. As a result, training policies vary dramatically.
In California’s IHSS program, clients are in charge of hiring, managing and training their own caregivers. The program stands out because of its sheer size — it is the nation’s largest publicly funded home care program – and because such a high percentage of caregivers are relatives directly employed by the clients rather than agencies, said Abby Marquand, director of policy research for the Paraprofessional Healthcare Institute.
“It is a lot easier to ensure a minimum level of training if the person is employed through an agency,” she said.
IHSS was never intended to be a medical program. The caregivers are distinct from visiting nurses and the certified home health aides often dispatched after a hospital stay. IHSS caregivers are not certified or licensed and are hired to do personal care and household tasks.
But more than a quarter of IHSS clients are 80 or over, and many have chronic health conditions or dementia. In these and other cases, caregivers can end up providing basic medical care–helping to administer insulin shots, manage other medication or dress wounds, for instance.

Charles Massengale needs to be supervised when he eats because he has a tendency to fall asleep and forget to eat (Photo by Heidi de Marco).
When such “paramedical” services are needed by individual clients, IHSS caregivers are required to get instruction and approval from a health care professional. But the state doesn’t sponsor the training or pay caregivers more for getting it. Only 12 percent of clients have caregivers who have received it.
Eileen Carroll, deputy director of the California Department of Social Services, which oversees IHSS, said the program doesn’t have a lot of training requirements because it was set up to give clients the choice of how they want their care delivered.
For caregivers who want it, the state offers comprehensive voluntary training information online on topics such as fall prevention and use of medical equipment, she said.
Carroll said many people are fully able to direct their own care and supervise their caregivers, but some aren’t. “Our task is how to work harder to support those who have greater need,” she said.
Oliver Massengale, for example, can’t depend on his brother to tell him what he wants or needs — Charles no longer talks much. “Because of the nature of the injuries and his different ailments, he could never train,” Oliver said. “He can’t even take care of himself.”
The situation worsened recently because Charles’ health insurance plan changed, and he no longer is being visited by a nurse. So every day Oliver sits inches from Charles, checking his blood pressure and blood sugar and coaching him step-by-step on how to inject insulin into his own arm.
“Hold the back of that needle up,” he told Charles on a recent day. “Put it in right there. Now pump the medicine in. Good, good.”
When he heard about a training class in Los Angeles, Oliver said he jumped at the chance.
“If I’d had this class in advance, it would have made it a lot easier,” he said.
A sensitive matter
Whether or not to require training for those who care for California’s 490,000 low-income elderly and disabled home care clients is a sensitive political — and personal — issue.
Carroll said the state is in a tough situation. Training is a positive thing, she said, “but you have a very strong adult disabled community in this program who … oppose any mandatory training.”
Many disability rights advocates say a training mandate would make it more difficult for IHSS consumers to find caregivers, chip away at clients’ autonomy and drain resources from the program.
“The idea of choice is really paramount,” said Deborah Doctor, legislative advocate at Disability Rights California. “Anything that puts a requirement that erodes that choice is a problem.”

Frances Chuc brushes her husband’s hair. Jorge Chuc has been paralyzed for more than 30 years and needs full-time care from his wife (Photo by Heidi de Marco/KHN).
Relatives, who make up nearly three-quarters of paid IHSS caregivers, often say they know what is best for their loved ones. And clients are inclined to trust family members and say they can instruct them on what they need.
“A mother who has been taking care of a child for 20 or 30 or 40 years doesn’t need mandatory training on how to take care of that person,” Doctor said.
Training should be made available to those who want it, but should be entirely voluntary, said Nancy Becker Kennedy, who was paralyzed in a diving accident 40 years ago.
“There is no one size fits all,” said Becker Kennedy, who founded IHSS Consumers Union, a group that advocates for both consumers and workers. “The population is much too diverse to mandate anything across the board.”
Many other clients agree. Sheela Gunn-Cushman, who is blind, diabetic and has mild cerebral palsy, lives with roommates in San Lorenzo, Calif., with the help of an IHSS caregiver whom she trained herself.
“I don’t feel like anyone is capable of training a [caregiver] about what I need better than I do,” she said. “I am capable of telling them what I need.”
A union that represents caregivers, however, sees advantages to a minimum level of training.
SEIU-United Healthcare Workers West proposed a statewide initiative last year that would have required 75 hours of training, but the union didn’t get enough signatures to put the measure on the ballot. SEIU plans to try again for the 2016 ballot.
Requiring training would “save lives,” said Loretta Jackson, who serves on the union’s executive board and is an IHSS caregiver in Sacramento. It would also reduce the risk of injuries to caregivers, she added.
Jackson cares for her sister, who was left partially paralyzed by a stroke 15 years ago. When Jackson first started, she had to call paramedics every few weeks because her sister would fall. Once, Jackson said, her sister took too many pills and started shaking violently.
“I didn’t know what to do,” she said. “I started panicking.”
Other caregivers tell similar stories.
Ariana Ramos, 28, who is taking a training class, said a paralyzed client got a bed sore after sleeping in his wheelchair. Ramos thought it would heal on its own, but it just got worse.
“Now I know that we need to keep it covered up,” said Ramos, who lives in South Gate. “Now I know about bacteria and all the things that could get in a bed sore.”

Frances Chuc takes a break after a morning of taking care of her paraplegic husband. She says taking care of her husband is daunting, but her previous experience as a caregiver has been helpful (Photo by Heidi de Marco/KHN).
Caregivers without any medical background or training may not know when to call 911 or how to recognize a heart attack or stroke, said Frances Chuc, who takes care of her paralyzed husband at their home in South Gate and was trained as a nurse aide before she met him. “That person could die in their hands.”
A little bit of training can go a long way, said Joanne Spetz, director of UC San Francisco’s newly created Health Workforce Research Center. It can help caregivers recognize when their clients are having bad reactions to medications, for instance, or help them safely lift a person to avoid falls.
Training can also reduce turnover in a field that has low job retention, said Marquand of the Paraprofessional Healthcare Institute.
Several states are experimenting with different models of training. Washington State, for example, began requiring 75 hours of training for home caregivers in 2012.
It doesn’t make sense that caregivers in the home require less training nationwide than caregivers in nursing homes, said Charissa Raynor, executive director of the SEIU Healthcare NW Training Partnership, which trains 40,000 providers annually. (Certified aides in nursing homes are required by the federal government to have 75 hours of training.)
The Washington initiative, Raynor said, will help professionalize the workforce, reduce on-the-job injuries and lead to better care.
But not everyone has been happy with the new mandate.
“There are a lot of folks who just want to be a caregiver in someone’s home,” said Betty Schwieterman, director of systems advocacy at Disability Rights Washington. “They are not on a career path.”
Grants From The Government
The debate over mandatory training is far from resolved. But in the meantime, the federal government is putting money into pilot training efforts in various states.
Through the Affordable Care Act, it has awarded about $15 million in grants to California and five other states to recruit and train qualified caregivers for the elderly and disabled populations. Classes started in 2011 in cities throughout the state, including San Francisco, Anaheim and Walnut.
The class Massengale attended is part of a separate federal grant of nearly $12 million given to the California Long-Term Care Education Center in Los Angeles. The center is training about 6,000 IHSS caregivers in Los Angeles, San Bernardino and Contra Costa counties.
An early evaluation of the program by UC San Francisco researchers shows that clients with trained providers are less likely to go to the emergency room or be admitted to a hospital than those with untrained providers.
Corinne Eldridge, who runs the program, said trained caregivers can play an important role on a client’s health care team. “They can be the eyes and the ears in the home … and communicate back to the health care provider,” she said.

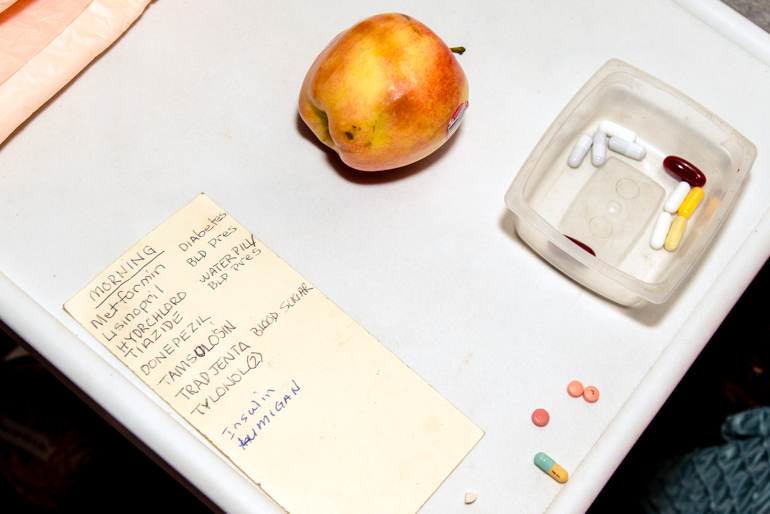
Charles Massengale takes his medicine one at a time during meals (Photo by Heidi de Marco/KHN).
At a recent session in Compton, about two dozen caregivers gathered in a classroom at the public library, their binders of training materials spread out before them. The topic of the day was preventing bed sores and controlling infections.
The teacher, nurse Lori Picou, asked the class about the signs and symptoms of infection. The students yelled out answers: Redness. Fever. Fluid or discharge.
One offered a story about a bruise that swelled up like a basketball. Another said her paralyzed son was sweating so much that she had to repeatedly change his shirt.
Picou reminded the group to wash their hands frequently. “It is one of the most important things an individual can ever do to help control infection,” she said.
Oliver Massengale, who is in the class, said he is feeling a little bit more confident about keeping his brother safe. “The more I learn, the better I am to cope with this,” he said.
But being a caregiver for someone with so many health conditions is still scary to him.
“As I come down those stairs,” he said, “I am saying a prayer and just hoping that everything is all right when I get to the bottom.”
KHN’s coverage of California is supported in part by the Blue Shield of California Foundation and The California Endowment. KHN also receives support from The SCAN Foundation for coverage of aging and long-term care issues.