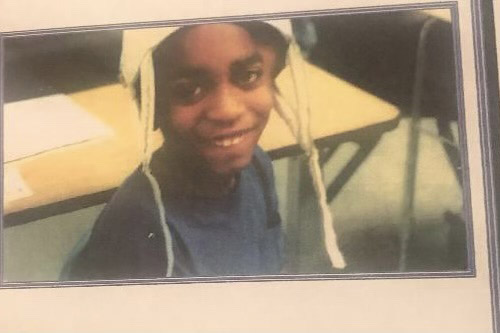
Oronde McClain was struck by a stray bullet on a Philadelphia street corner when he was 10.
The bullet shattered the back of his skull, splintering it into 36 pieces. McClain’s heart stopped, and he was technically dead for two minutes and 17 seconds.
Although a hospital team shocked him back to life, McClain never fully recovered. Doctors removed half his skull, replacing it with a gel plate, but shrapnel remains.
The shooting left him in a coma for seven weeks and in a wheelchair for nearly two years. School bullies magnified his pain, laughing at his speech and the helmet he wore to protect his brain. McClain said he repeatedly attempted suicide as a teenager. He remains partly paralyzed on his right side and endures seizures and post-traumatic stress disorder.
“People who die, they get funerals and balloon releases,” said McClain, now 33. “Survivors don’t get anything.”

Yet the ongoing medical needs of gun violence survivors and their families are vast.
In the year after they were shot, child and adolescent survivors were more than twice as likely as other kids to experience a pain disorder, said Zirui Song, an associate professor of health care policy and medicine at Harvard Medical School and the co-author of a new study in Health Affairs. The shooting survivors in the study — age 19 and younger — were found to be 68% more likely than other kids to have a psychiatric diagnosis and 144% as likely to develop a substance use disorder.
Across the United States, firearm injuries were the leading cause of death for people ages 1 to 19 in 2020 and 2021, according to the Centers for Disease Control and Prevention. More than 48,000 Americans of all ages were killed by firearms in 2022. And an average of about 85,000 Americans survive firearm injuries every year.
“The public hears about mass shootings and the number of people who died,” Song said. “The population of people affected by firearm violence is much larger than deaths alone.”
Most Americans say they or a family member has experienced gun violence, including witnessing a shooting, being threatened by a person with a gun, or being shot, according to a KFF survey.
“We are now a nation of survivors, and we have an unmet obligation to help families and communities heal, both physically and emotionally,” said Megan Ranney, dean of the Yale School of Public Health.
Being shot added an average of $35,000 to the health care costs of each young person studied, compared with the expenses of those who weren’t shot. The more serious the injury, the greater the cost and extent of medical complications, according to the study, based on data from employer-sponsored health insurance plans.
Although McClain’s mother had health insurance through her employer, the plan did not cover the cost of his wheelchair. Insurance didn’t pay for dance or theater classes, which his therapists recommended to improve his speech and movement. Although his grandparents helped pay the medical bills, his family still held fundraisers to cover additional out-of-pocket costs.
The study is one of the first to assess the effects of a child’s shooting on the entire family, said Ranney, who was not involved in the research.
Psychiatric disorders were 30% more common among the parents of the gun-injured children, compared with parents of uninjured kids. Their mothers made 75% more mental health visits than other moms.
Ranney noted that caregivers of shooting survivors often neglect their own needs. In the study, parents and siblings of the injured children made fewer visits for their own routine medical care, lab tests, and procedures.
Doctors can now save most gunshot victims, said Jessica Beard, a trauma surgeon at Temple University Hospital who was not involved in the study.
“We have more experience with bullet wounds than even many battlefield surgeons,” said Beard, who is also director of research for the Philadelphia Center for Gun Violence Reporting. “Surgeons from the military will get stationed at hospitals in Philadelphia to learn how to do combat surgery.”
Survivors of gunshot wounds often need continuing care from physical therapists, occupational therapists, makers of prosthetics, and others, which can pose additional hardships for rural residents, who may need to travel long distances multiple times a week for specialized services. Even in major U.S. cities, the hospitals and health systems best equipped to treat shooting survivors may be out of range for families who rely on public transportation.
Using public transportation would have been especially difficult when McClain was in a wheelchair. He said he feels lucky that his grandfather could drive him to the hospital for the first couple of years after his shooting. Later, when McClain could walk, he took two buses and a subway to the hospital. Today, McClain drives himself to get care and receives health insurance through his employer.
The psychological damage from child shootings may be even greater than the study indicates, Ranney said. Negative attitudes surrounding mental illness may have prevented some patients from acknowledging they’re depressed, so their struggles weren’t recorded in doctors’ notes or payment records, she said. Likewise, children afraid of punishment may not have told their doctors about illegal substance use.
McClain said he saw a therapist only once or twice. “I would scream at the doctors,” McClain said. “I said, ‘Don’t tell me you know how I feel, because you don’t understand.’”
Yet McClain has found purpose in his experience.
Last year, he co-produced a documentary called “They Don’t Care About Us, or Do They?” with the Philadelphia Center for Gun Violence Reporting, where he works. In the film, young survivors talk about wearing hoodies to hide their scars, navigating the world in a wheelchair, and combating infertility caused by their injuries. McClain is now working to improve news coverage of gun violence by creating a directory of shooting survivors willing to share their stories.
“My therapy is helping people,” he said. “I have to wake up and save somebody every day.”
Survivors are the forgotten victims of the nation’s gun violence epidemic, McClain said. Many feel abandoned.
“They push you out of the hospital like you have a normal life,’’ McClain said. “But you will never have a normal life. You are in this club that you don’t want to be in.”
[Correction: This article was updated at 9:30 p.m. ET on Nov. 6, 2023, to remove a passage in Jessica Beard’s quote.]







