Computers are everywhere in medicine. If you have an operation, your surgeon might study the best practices online before the procedure. If you are diagnosed with a difficult-to-treat cancer, chances are your doctor will use an online database to find an appropriate clinical trial. And, if you develop a rash, you’ll probably use the Internet to find out what it might be.
Donald Lindberg, the outgoing director of the National Institutes of Health National Library of Medicine, had a hand in making these resources widely available. Since he joined the NLM in 1984, he saw the promise in putting research online so that doctors could have the latest medical advancements at their fingertips. And he wanted that same option for patients as they’ve become increasingly engaged in navigating their own care.
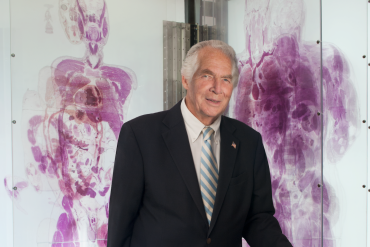
Dr. Donald Lindberg. (Photo courtesy of National Institutes of Health)
“When I first arrived at NLM, I didn’t come prepared to change anything, but technology was changing all around all of us,” Lindberg said. “We’ve had to make major changes or else we would have become obsolete.” The National Library of Medicine, which is the world’s largest medical library, was founded in the 1800s and initially sent out a monthly guide to medical research. As technology has evolved, so have the methods the library uses to disseminate information to patients and providers.
He still remembers his early days at NIH, when information-sharing technology involved phone companies and point-to-point transmissions. But the advent of computers and the World Wide Web changed all of that.
Lindberg, who pioneered the first use of computers in medicine in the 1960s, was involved during his 30-year tenure with almost every government-funded sorting initiative of new and old medical information — the 1998 creation of Medline Plus for consumers to find out general medical information; the 1997 creation of Clinicaltrials.gov, the largest global registry for these types of studies; and the management and installment of Visible Humans, an online library of digital images based on the anatomy of a man and woman.
Lindberg, who retired April 1, recently spoke with KHN’s Lisa Gillespie about his NLM experience and what he thinks is next on the horizon. An edited transcript of their conversation follows.
Q: What are some of the biggest changes that took place during your time at NLM and shaped the experience of being a doctor or patient?
A: The introduction of computer interpretation of EKGs in the study of the heart was one piece of pavement in the road of success for computers. That was greeted pretty much with support from patients and doctors, though doctors were [also] concerned in making sure the stuff was right. I would say most are not experts [in interpreting this technology], especially in the case of general practitioners. It was a big deal for a computer to do that, and it was rapidly accepted.
Q: You were involved in the creation and roll out of many systems to help doctors and patients. Which ones have made the greatest impact?
A: Medline Plus, a database that tells you things like what chemicals and drugs get into mother’s milk, has had a lot of influence. If you’re lactating, it is of great interest. The major change in our whole field was Human Genome Project. That project has produced millions and even billions of facts that would only achieve meaning if they were put together to answer questions, [which was done through Medline Plus].
A very current one is clinicaltrials.gov. [The concept] started at the National Institutes of Health, and even there, if you asked “how many clinical trials are going on?” there was no answer. There wasn’t even a list. We were surprised to discover that. … Everyone agreed there should be records [of trials]. In Israel, for instance, they saw what we were doing and said it was going to take too much money to do it [themselves], so they started putting their records in our system. Clinicaltrials.gov now has 150,000 trials [listed in the global database].
Q: As NLM created and implemented computer applications, did health care providers shape what information was shared and how technology was used?
A: At one point, I was trying to do things the nurses would like. The chief of nursing came to me and said the computer was a wonderful thing. I asked her what she liked about it, and she said, “well, it’ll give me an alphabetized list of names on the ward.” That’s not a great accomplishment, but it’s what they wanted. We tried to keep our eyes out for things like that.
Q: What are the biggest technological innovations you’ve seen?
A: The idea of telemedicine is a very powerful one, and it’s been with us for a long time. Once we get improved gear [for its use], there will be a new application that I couldn’t have thought of. Take tele-dermatology. There aren’t enough experts. … So the basic idea is that once you have digital cameras, you send [case information] to an expert who will look at it and give an opinion. A dermatologist told me once about a patient who had obvious dermatitis problems and had spent five years going to doctors who couldn’t treat it. The guy was unemployable because his condition was so severe that he couldn’t move around. And it got cured [using telemedicine].
Q: What are your predictions for the future? Especially at the NLM?
A: The idea of the informed patient will dominate changes. You can’t underestimate patients. [Now] versus when I got started … they’re willing to participate in medical-decision making. Back then, patients didn’t want an active role in their own management. Smart doctors now encourage it. That will make a big difference. Now they [are starting to] understand prevention … and they’ll understand end-of-life care. How aggressive the treatment is should be based on the patient’s wishes, but they have to understand [the choices].






