Medicare launched a website aimed at helping families choose a hospice — but experts say it doesn’t help very much.
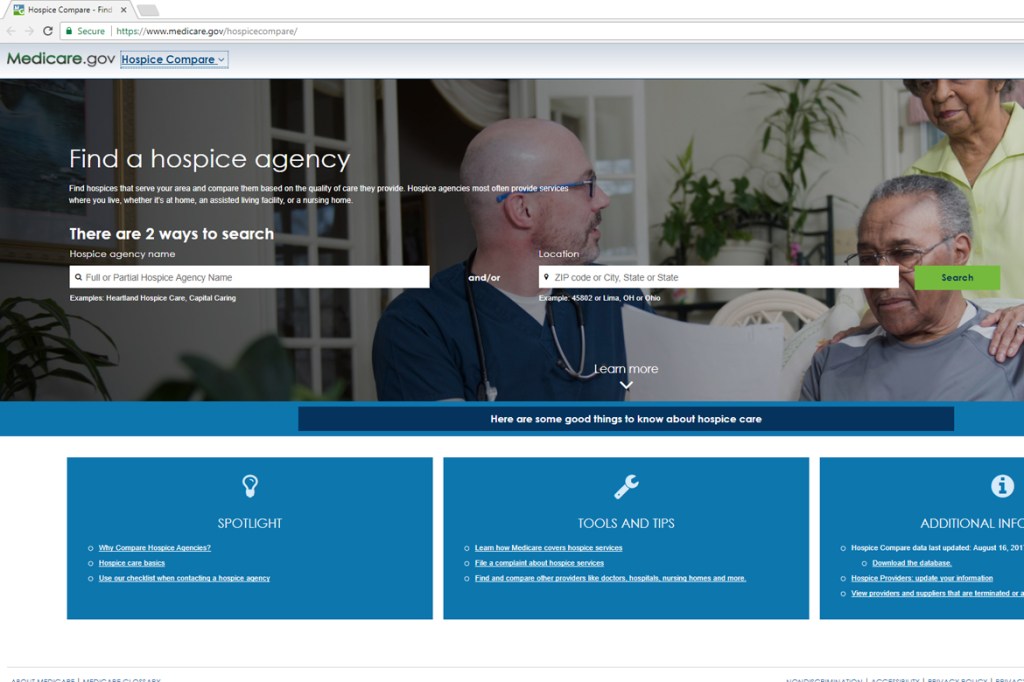
The Centers for Medicare & Medicaid Services this week released Hospice Compare, a consumer-focused website that lets families compare up to three hospice agencies at a time, among 3,876 nationwide. Following similar websites for hospitals and nursing homes, the site aims to improve transparency and empower families to “take ownership of their health,” according to a press release.
Through the website, families can see how hospices performed in seven categories, including how many patients were screened for pain and breathing difficulties, and how many patients on opioids were offered treatment for constipation.
But the measurements of quality, which are self-reported by hospices, have limited utility, some experts say. Over three-quarters of hospices scored at least 91 percent out of 100 on six of the seven categories, a recent paper in Health Affairs found. Because so many hospices reported high marks, there is “little room” for using these metrics to measure hospice quality, argued the authors, led by Dr. Joan Teno at the University of Washington.
The Hospice Compare grades are based on hospices reporting whether they followed a specific process, such as screening for pain when the patient arrives. This type of metric may lead staff to just check a box to indicate they completed the desired process, resulting in high grades for everyone, which is not helpful for consumers or for quality improvement, the authors wrote.
Meanwhile, Teno’s other research has found troubling variation in hospice quality, measured by how often hospice staff visit a patient when death is imminent.
“It’s nice that they’re at least beginning to be concerned about hospice quality,” said Dr. Joanne Lynn of the Altarum Institute, a longtime hospice physician and researcher, of CMS’ new website. But “at the present time, it’s of pretty limited value.”
Lynn said people trying to choose a hospice would be better helped by other kinds of information, such as the average caseload for hospice staff; what percentage of patients are discharged alive; and whether the hospice predominantly serves nursing home patients or devotes significant resources to at-home care.
The Hospice Compare website also doesn’t say how often hospices run awry of federal regulations: Inspection reports, which contain verified consumer complaints as well as problems uncovered during routine inspections, are not part of the website, as they are for nursing homes.
Recent hospice inspection reports may be hard to find. Until a recent federal rule change, hospices could go as long as six years without being inspected. By 2018, CMS requires states to increase the frequency to once every three years.
Common quality measures for hospitals and nursing homes, such as mortality rates, don’t translate well to the hospice setting, where people are expected to die, Lynn noted.
Although Hospice Compare is “skeletal” at the moment, Lynn said, it does enable families to search which hospices are near them, and find the hospice’s phone number to start asking questions.
“I’m hoping that it continues to improve over time,” as CMS’ other consumer-focused websites have, she said.
Next year, CMS plans to add family ratings of hospices, including how timely hospice staff were when a patient needed help. CMS is also collecting data on the number of staff visits a patient received in the final week before death. That information should be made public in late 2018, a CMS spokesman said Wednesday.
KHN’s coverage of end-of-life and serious illness issues is supported by The Gordon and Betty Moore Foundation and its coverage related to aging & improving care of older adults is supported by The John A. Hartford Foundation.