Latest KFF Health News Stories
A Mom’s $97,000 Question: How Was Her Baby’s Air-Ambulance Ride Not Medically Necessary?
There are legal safeguards to protect patients from big bills like out-of-network air-ambulance rides. But insurers may not pay if they decide the ride wasn’t medically necessary.
After Appalachian Hospitals Merged Into a Monopoly, Their ERs Slowed to a Crawl
Ballad Health was granted the nation’s largest state-sanctioned hospital monopoly in 2018. Since then, its emergency rooms have become more than three times as slow.
Journalists Track Efforts to Curb the Opioid Crisis and Put Catholic Hospitals Under the Scope
KFF Health News and California Healthline staff made the rounds on national and local media in recent weeks to discuss their stories. Here’s a collection of their appearances.
Health Workers Fear It’s Profits Before Protection as CDC Revisits Airborne Transmission
Four years since the covid pandemic emerged, health care workers want rules that protect them during outbreaks. They worry the CDC is repeating past mistakes as it develops a crucial set of guidelines for hospitals, nursing homes, prisons, and other facilities that provide health care.
Cuando tu cobertura de salud dentro de la red… simplemente se esfuma
los contratos de las aseguradoras con médicos, hospitales y farmacéuticas (o sus intermediarios, los llamados administradores de beneficios farmacéuticos) pueden cambiar abruptamente de la noche a la mañana.
How Your In-Network Health Coverage Can Vanish Before You Know It
One of the most unfair aspects of medical insurance is this: Patients can change insurance only during end-of-year enrollment periods or at the time of “qualifying life events.” But insurers’ contracts with doctors, hospitals, and pharmaceutical companies can change abruptly at any time.
En 2022, el año más reciente del que se dispone de datos, 7,385 californianos murieron por sobredosis relacionadas con opioides, de los cuales el 88% involucró fentanilo, un opioide sintético que puede ser 50 veces más potente que la heroína.
VIP Health System for Top US Officials Risked Jeopardizing Care for Soldiers
The historically troubled White House Medical Unit is just one part of a government health system that gives VIP care to top officials, military officers, military retirees, and families. Pentagon investigators say some were prioritized over rank-and-file soldiers.
Biden Team, UnitedHealth Struggle to Restore Paralyzed Billing Systems After Cyberattack
The cyberattack on a unit of UnitedHealth Group’s Optum division is the worst on the health care industry in U.S. history, hospitals say. Providers struggling to get paid for care say the response by the insurer and the Biden administration has been inadequate.
Operating in the Red: Half of Rural Hospitals Lose Money, as Many Cut Services
A recent report finds half of America’s rural hospitals are losing money, and many are struggling to stay open. Researchers and advocates worry the hospitals’ financial spiral will have immediate and long-term health effects on their communities.
Why Hospitals in Many States With Legal Abortion May Refuse To Perform Them
Many states that tout themselves as protectors of reproductive health care, including California, Michigan and Pennsylvania, have little-noticed laws on the books protecting hospitals that refuse to provide it. The laws shield at least some hospitals from liability for not providing care they object to on religious grounds, leaving little recourse for patients. The providers — many of them […]
California Hospitals, Advocates Seek Stable Funding to Retain Behavioral Health Navigators
California has supported expanded use of medications in the fight against opioid use disorder and overdose deaths. But hospitals and addiction treatment advocates say the state needs to secure ongoing funding if it wants more behavioral health workers to guide patients into long-term treatment.
A Government Video Would Explain When Abortion Is Legal in South Dakota
South Dakota allows doctors to terminate a pregnancy only if a patient’s life is in jeopardy. Lawmakers say a government-created video would clarify what that exception actually means.
Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight
Sky-high bills from air-ambulance providers have sparked complaints and federal action in recent years. But a rural Tennessee resident fell through the cracks of billing protections — and a single helicopter ride could cost much of her estate’s value.
What the Health? From KFF Health News: Alabama Court Rules Embryos Are Children. What Now?
In a first-of-its-kind ruling, the Alabama Supreme Court has determined that embryos created for in vitro fertilization procedures are legally people. The decision has touched off massive confusion about potential ramifications, and the University of Alabama-Birmingham has paused its IVF program. Meanwhile, former President Donald Trump is reportedly planning to endorse a national 16-week abortion ban, while his former administration officials are planning further reproductive health restrictions for a possible second term. Lauren Weber of The Washington Post, Rachana Pradhan of KFF Health News, and Victoria Knight of Axios join KFF Health News’ Julie Rovner to discuss these issues and more. Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too.
In California, Faceoff Between Major Insurer and Health System Shows Hazards of Consolidation
Even as Anthem Blue Cross and University of California Health announced a contract agreement this month, analysts say patients are increasingly at risk of being affected by such disputes.
The Powerful Constraints on Medical Care in Catholic Hospitals Across America
The expansion of Catholic hospitals nationwide leaves patients at the mercy of the church’s religious directives, which are often at odds with accepted medical standards.
In Fight Over Medicare Payments, the Hospital Lobby Shows Its Strength
Medicare pays hospitals about double what it pays other providers for the same services. The hospital lobby is fighting hard to make sure a switch to “site-neutral payments” doesn’t become law.
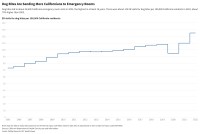
A Record Number of Californians Are Visiting Emergency Rooms for Dog Bites
There were nearly 50,000 emergency room visits for dog bites in California in 2022. The rate of such visits per capita is up about 70% since 2005.
What the Health Care Sector Was Selling at the J.P. Morgan Confab
When bankers and investors flocked to San Francisco for the largest gathering of health care industry investors, the buzz was all about artificial intelligence, the next hit weight-loss drug, and new opportunities to make money through nonprofit hospitals.