The marketing pitches are bold and arriving fast: Invest opioid settlement dollars in a lasso-like device to help police detain people without Tasers or pepper spray. Pour money into psychedelics, electrical stimulation devices, and other experimental treatments for addiction. Fund research into new, supposedly abuse-deterrent opioids and splurge on expensive, brand-name naloxone.
These pitches land daily in the inboxes of state and local officials in charge of distributing more than $50 billion from settlements in opioid lawsuits.
The money is coming from an array of companies that made, sold, or distributed prescription painkillers, including Johnson & Johnson, AmerisourceBergen, and Walgreens. Thousands of state and local governments sued the companies for aggressively promoting and distributing opioid medications, fueling an epidemic that progressed to heroin and fentanyl and has killed more than half a million Americans. The settlement money, arriving over nearly two decades, is meant to remediate the effects of that corporate behavior.
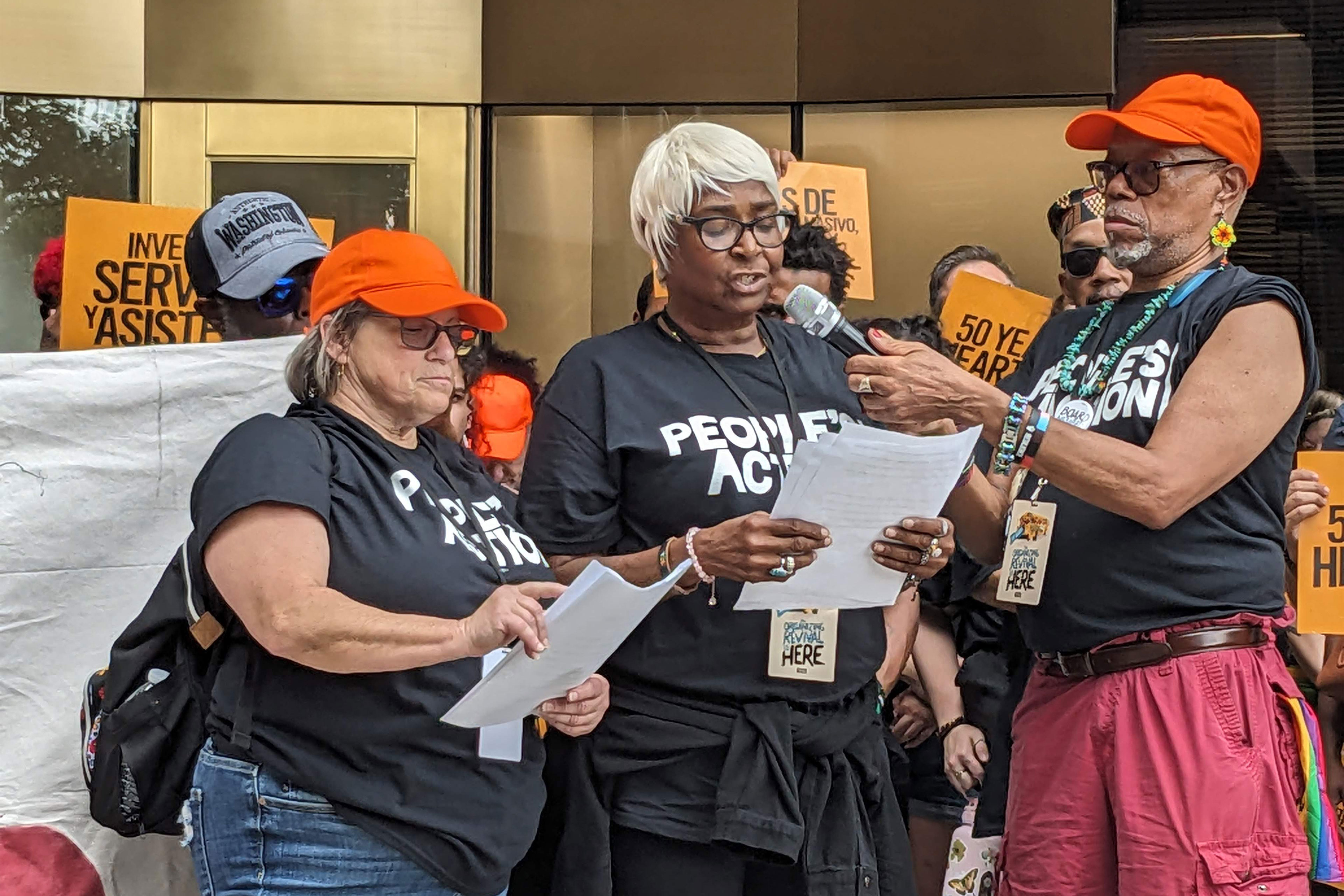
But as the dollars land in government coffers — more than $4.3 billion as of early November — a swarm of private, public, nonprofit, and for-profit entities are eyeing the gold rush. Some people fear that corporations, in particular — with their flashy products, robust marketing budgets, and hunger for profits — will now gobble up the windfall meant to rectify it.
“They see a cash cow,” said JK Costello, director of behavioral health consulting for the Steadman Group, a firm that is being paid to help local governments administer the settlements in Colorado, Kansas, Oregon, and Virginia. “Everyone is interested.”
Costello receives multiple emails a week from businesses and nonprofits seeking guidance on how to apply for the funds. To keep up with the influx, he has developed a standard response: Thanks, but we can’t respond to individual requests, so here’s a link to your locality’s website, public meeting schedule, or application portal.
KFF Health News obtained email records in eight states that show health departments, sheriffs’ offices, and councils overseeing settlement funds are receiving a similar deluge of messages. In the emails, marketing specialists offer phone calls, informational presentations, and meetings with their companies.
Alabama Attorney General Steve Marshall recently sent a letter reminding local officials to vet organizations that reach out. “I am sure that many of you have already been approached by a variety of vendors seeking funding for opioid initiatives,” he wrote. “Please proceed with caution.”
Of course, not all marketing efforts should prompt concern. Emails and calls are one way people in power learn about innovative products and services. The country’s addiction crisis is too large for the public sector to tame alone, and many stakeholders agree that partnering with industry is crucial. After all, pharmaceutical companies manufacture medications to treat opioid addiction. Corporations run treatment facilities and telehealth services.
“It’s unrealistic and even harmful to say we don’t want any money going to any private companies,” said Kristen Pendergrass, vice president of state policy at Shatterproof, a national nonprofit focused on addiction.
The key, agree public health and policy experts, is to critically evaluate products or services to see if they are necessary, evidence-based, and sustainable — instead of flocking to companies with the best marketing.
Otherwise, “you end up with lots of shiny objects,” Costello said.
And, ultimately, failure to do due diligence could leave some jurisdictions holding an empty bag.
Take North Carolina. In 2022, state lawmakers allotted $1.85 million of settlement funds for a pilot project using the first FDA-approved app for opioid use disorder, developed by Pear Therapeutics. There were high hopes the app would help people stay in treatment longer.
But less than a year later, Pear Therapeutics filed for bankruptcy.
The state hadn’t paid the company yet, so the money isn’t lost, according to the North Carolina Department of Health and Human Services. But the department and lawmakers have not decided what to do with those dollars next.
$1 Million for Drug Disposal Pouches
Jason Sundby, CEO of Verde Environmental Technologies, said the Deterra pouches his company sells are a low-cost way to prevent expensive addictions.
Customers place their unused medications in a Deterra pouch and add water, deactivating the drugs before tossing them, ensuring they cannot be used even if fished out of the trash. A medium Deterra pouch costs $3.89 and holds 45 pills.
The goal is to “get these drugs out of people’s homes before they can be misused, diverted, and people start down the path of needing treatment or naloxone or emergency room visits,” Sundby said.
Sundby’s company ran an ad about spending settlement dollars on its product in a National Association of Counties newsletter and featured similar information online.
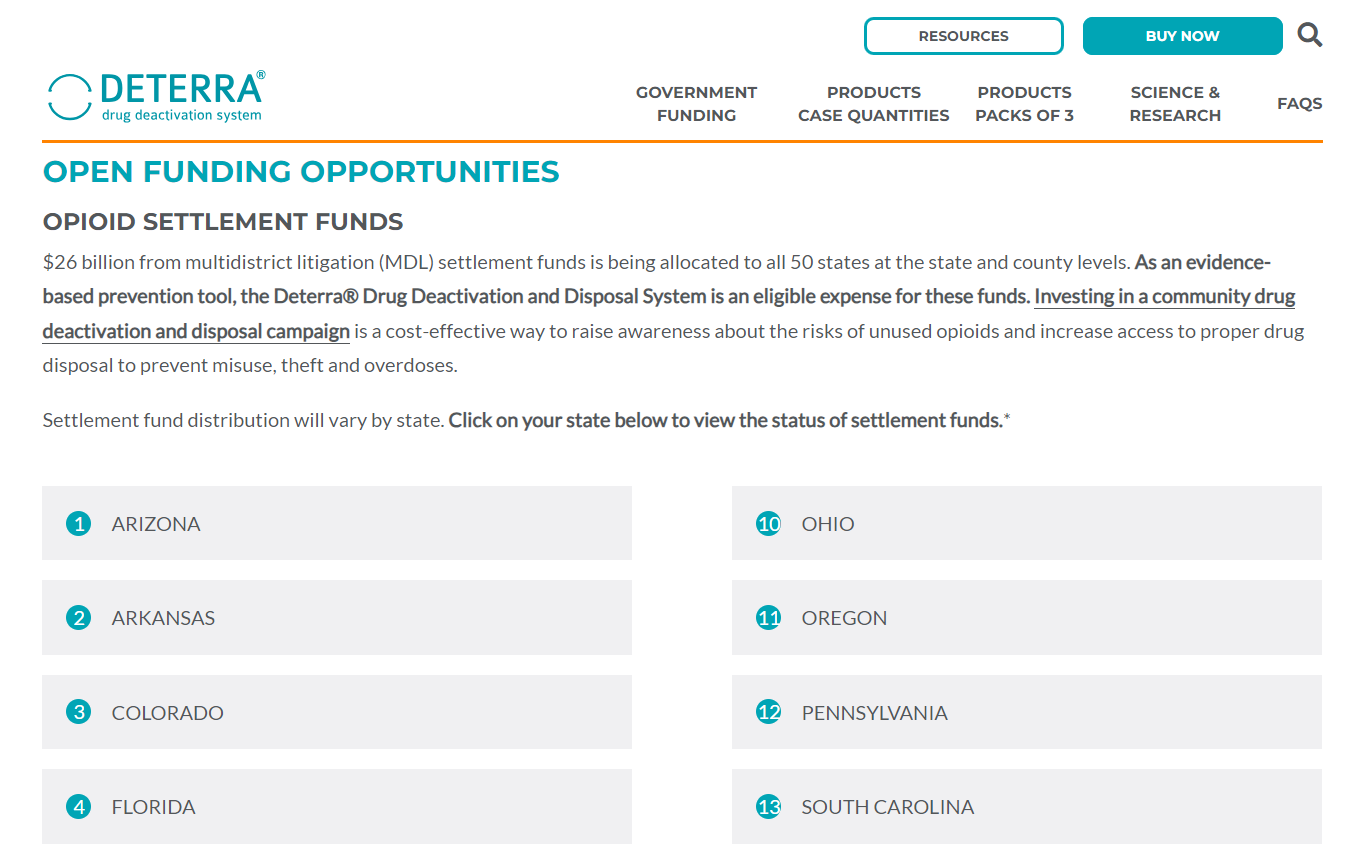
It may be paying off, as Deterra is set to receive $1 million in settlement funds from the health department in Delaware County, Pennsylvania, and $12,000 from the sheriff’s office in Henry County, Iowa. The company also has partnerships with St. Croix and Milwaukee counties in Wisconsin, and is working on a deal in Connecticut.
Several other companies with similar products have also used their product sites to urge jurisdictions to consider the settlements as a funding stream — and they’re seeing early success.
DisposeRx makes a drug deactivation product — its version costs about a dollar each — and received $144,000 in South Carolina for mailing 134,000 disposal packets to a program that educated high school football players, coaches, and parents about addiction.
SafeRx makes $3 pill bottles with a locking code to store medications and was awarded $189,000 by South Carolina’s opioid settlement council to work with the Greenville County Sheriff’s Office and local prevention groups. It also won smaller awards from Weld and Custer counties in Colorado.
None of the companies said they are dependent on opioid settlements to sustain their business long-term. But the funds provide a temporary boost. In a 2022 presentation to prospective investors, SafeRx called the opioid settlements a “growth catalyst.”
Critics of such investments say the products are not worthwhile. Today’s crisis of fatal overdoses is largely driven by illicit fentanyl. Even if studies suggest the companies’ products make people more likely to safely store and dispose of medications, that’s unlikely to stem the record levels of deaths seen in recent years.
“The plausible mechanism by which they would even be able to reduce overdose is a mystery because prescription medications are not driving overdose,” said Tricia Christensen, policy director with the nonprofit Community Education Group, which is tracking settlement spending across Appalachia.
Safe storage and disposal can be accomplished with a locking cabinet and toilet, she said. The FDA lists opioids on its flush list for disposal and says there is no evidence that low levels of the medicines that end up in rivers harm human health.
But Milton Cohen, CEO of SafeRx’s parent company, Caring Closures International, said keeping prescription medicines secure addresses the root of the epidemic. Fentanyl kills, but often where people start, “where water is coming into the boat still, is the medicine cabinet,” he said. “We can bail all we want, but the right thing to do is to plug the hole first.”

Products to secure and dispose of drugs also provide an opportunity for education and destigmatization, said Melissa Lyon, director of the Delaware County Health Department in Pennsylvania. The county will be mailing Deterra pouches and postcards about preventing addiction to three-quarters of its residents.
“The Deterra pouch is to me a direct correlation” to the overprescribing that came from pharmaceutical companies’ aggressive marketing, she added. Since the settlement money is to compensate for that, “this is a good use of the funds.”
Tools for Law Enforcement That Superheroes Would Envy
Other businesses making pitches for settlement funds have a less clear relationship to opioids.
Wrap Technologies creates tools for law enforcement to reduce lethal uses of force. Its chief product, the BolaWrap, shoots a 7½-foot Kevlar tether more than a dozen feet through the air until it wraps around a person’s limbs or torso — almost like Wonder Woman’s Lasso of Truth.

Terry Nichols, director of business development for the company, said the BolaWrap can be used as an alternative to Tasers or pepper spray when officers need to detain someone experiencing a mental health crisis or committing crimes related to their addiction, like burglary.
“If you want to be more humane in the way you treat people in substance use disorder and crisis, this is an option,” he said.
The company posts body camera footage of officers using BolaWrap on YouTube and says that out of 192 field reports of its use, about 75% of situations were resolved without additional use of force.
When officers de-escalate situations, people are less likely to end up in jail, Nichols said. And diverting people from the criminal justice system is among the suggested investments in opioid settlement agreements.
That argument convinced the city of Brownwood, Texas, where Nichols was police chief until 2019. It has spent about $15,000 of opioid settlement funds to buy nine BolaWrap devices.
“Our goal is to avoid using force when a citizen is in need,” said James Fuller, assistant police chief in Brownwood. “If we’re going to take someone to get help, the last thing we want to do is poke holes in them with a Taser.”
After Brownwood’s purchase, Wrap Technologies issued a press release in which CEO Kevin Mullins encouraged more law enforcement agencies to “take the opportunity afforded by the opioid settlement funds to empower their officers.” The company has also sent a two-page document to police departments explaining how settlement funds can be used to buy BolaWraps.
Language from that document appeared nearly word-for-word in a briefing sheet given to Brownwood City Council before the BolaWrap purchase. The council voted unanimously in favor.
But the process hasn’t been as smooth elsewhere. In Hawthorne, California, the police department planned to buy 80 BolaWrap devices using opioid settlement funds. It paid its first installment of about $25,000 in June. However, it was later informed by the state Department of Health Care Services that the BolaWrap is not an allowable use of these dollars.
“Bola Wraps will not be purchased with the Settlement Funds in the future,” Hawthorne City Clerk Dayna Williams-Hunter wrote in an email.
Carolyn Williams, a member of the advocacy group Vocal-TX, said she doesn’t see how the devices will address the overdose crisis in Texas or elsewhere.
Her son Haison Akiem Williams dealt with mental health and addiction issues for years. Without insurance, he couldn’t afford rehab. When he sought case management services, there was a three-month wait, she said. Police charged him with misdemeanors but never connected him to care, she said.
In February, he died of an overdose at age 47. His mother misses how he used to make her laugh by calling her “Ms. Carol.”
She wants settlement funds to support services she thinks could have kept him alive: mental health treatment, case management, and housing. BolaWrap doesn’t make that list.
“It’s heartbreaking to see what the government is doing with this money,” she said. “Putting it in places they really don’t need it.”







