States would be able to use federal funding to provide subsidies to people buying short-term health insurance policies, which typically don’t provide comprehensive coverage, under guidance released Monday by the Trump administration.
The new policy could begin taking effect in 2020. It would allow states to ask for waivers from Affordable Care Act provisions governing not only subsidies that help pay for premiums, but also the benefits insurers must include in plans offered on the federal marketplace to consumers buying their own coverage.
The announcement comes two weeks before the crucial midterm Election Day as health care tops voters’ list of concerns.
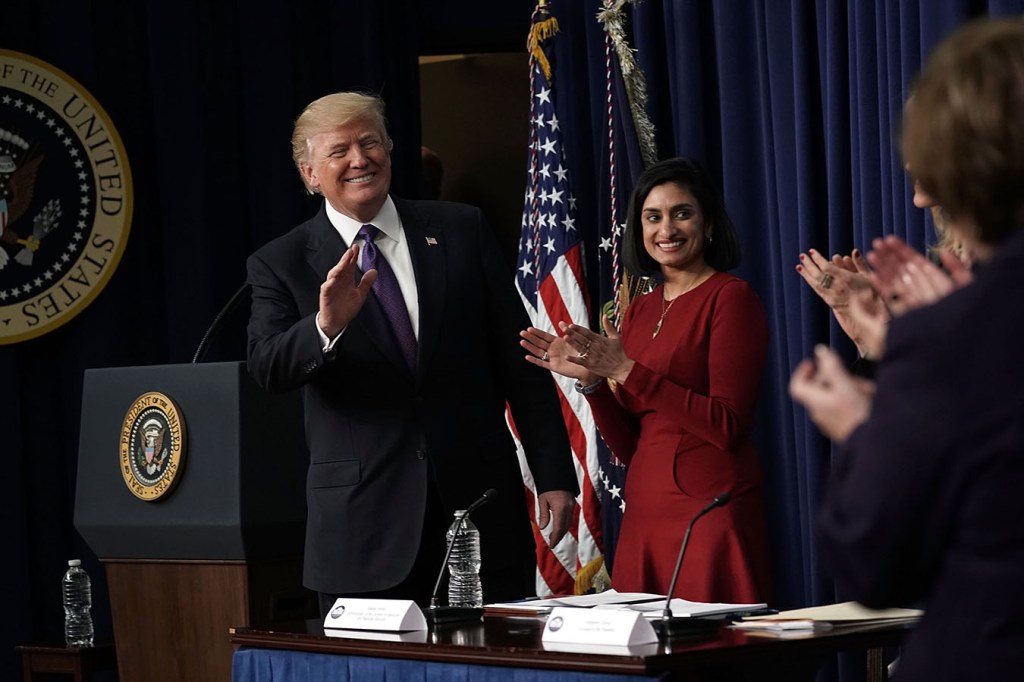
States were asking for more flexibility, said Seema Verma, administrator of the Centers for Medicare & Medicaid Services (CMS). This approach would allow the states “to provide consumers plan options that best meet their needs, while at the same time ensuring that those with preexisting conditions retain access to the same coverage as today,” she said.
Under the ACA, states can ask to reconfigure their insurance markets and rules. The Obama administration required any changes to provide the same comprehensive coverage as the health law and not result in fewer people enrolling or increasing costs for taxpayers.
Those guidelines hampered finding creative ways to expand coverage and lower costs, Verma said.
The new guidance substantially revises those Obama-era “guardrails,” allowing waivers so long as access to comprehensive plans remains.
“The big change is they no longer have to worry about making sure that people with preexisting conditions or high health care needs maintain enrollment in comprehensive coverage,” said Sabrina Corlette, research professor at the Center on Health Insurance Reforms at Georgetown University.
“The Trump administration looks like it’s willing to aggressively test the boundaries of the law when it comes to waivers. Whether that’ll stand up in court is very much open to question,” said Nicholas Bagley, a health law professor at the University of Michigan Law School.
Under Monday’s revised guidance, CMS is changing how it defines insurance sold on the ACA marketplaces in 2020 to include short-term or association health plans. These plans don’t have to follow all the Obamacare rules for eligibility and benefits. Short-term plans, for example, don’t have to be comprehensive and can exclude people with certain health conditions or charge them higher premiums. They can leave out coverage for mental health, prescription drugs or maternity care, for example.
Under President Barack Obama, such plans were limited to 90-day terms. The Trump administration this spring said short-term plans could be sold for up to a year and gave insurers the option to renew them for up to three years.
However, they cannot be sold through the health law marketplaces in 2019 and are not now eligible for federal premium subsidies for low-income customers.
Earlier in the year, the administration also approved a rule allowing businesses to band together in “associations” to buy health insurance to offer insurance to members. Critics fear that rule could expose consumers to coverage gaps or higher out-of-pocket costs because these plans would be classified as “large-group plans” and not have to meet some ACA requirements.
The changes unveiled on Monday do not affect people who get their coverage through their jobs.
Verma is using an Obamacare provision — so-called 1332 waivers — to dramatically reshape Obamacare, a health law she has repeatedly called on to be repealed by Congress.
She insisted that none of the changes would hinder people with preexisting conditions from buying or affording coverage. That concern has proven to be a potent campaign message for Democrats.
The new guidelines could increase enrollment for consumers who forgo coverage because of cost.
Under Monday’s proposal, states could also ask to change eligibility for subsidies under the ACA, perhaps to offer bigger amounts to younger adults — not necessarily tied to their income — as a way to drive them to buy coverage, said Verma.
States have struggled to attract younger adults to buy coverage in the Obamacare marketplaces. That age group is prized because it tends to have the lowest health risks and lowest costs, which helps balance the insurers’ risk pools and keep premiums from rising.
As expected, Obamacare opponents hailed the new guidance from CMS.
“Americans should have lower costs and more choices when it comes to health care, so the Trump administration has taken a good next step with the waiver process,” said Doug Badger, a visiting fellow for the conservative Heritage Foundation. “By removing even a few Obamacare restrictions, the administration has opened the door to more patient-friendly state innovation.”
Yet the guidance also moves the country back to an era when there was wide variation in insurance rules state to state, others noted.
“The ACA was passed in 2010 because states weren’t getting the job done,” said Corlette at Georgetown. “We had a patchwork of protections at the state level, 49 million uninsured and people being denied coverage because they had preexisting conditions.”
Analysts both inside and outside the government predict that the less expensive short-term plans would draw younger and healthier people from the ACA marketplaces, thus driving up premiums for those who remain.
Estimates on how many would do so and what the total effect on premiums would be varies widely. Verma said that earlier reports done by the administration indicated there would be only a modest effect on ACA premiums by increased enrollment in short-term plans.
Corlette said that remains unclear. The effect on premiums, she said, is unknown because no state has applied yet under the new guidance.
“The hypotheticals that are permissible under this could dramatically raise premiums for people with preexisting conditions, but it’s just too early to say,” she said.
Verma said several states have come to her asking to make changes in how they sell individual insurance, although she declined on a call with reporters to name the states.
The average health insurance rates for Obamacare plans are falling by 1 percent for 2019 — its first-ever drop, CMS announced earlier this month. But Verma said rates remain too high.
“In response to numerous requests from governments, the administration is giving states the flexibility they need to increase choices and combat high Obamacare premiums,” she said.
KHN chief Washington correspondent Julie Rovner contributed to this report.